People who are considering becoming a kidney donor must carefully weigh the potential risks and benefits of donating a kidney.
Although the surgery itself is often a major component of this decision, other factors such as medical risks, the cosmetic result, and socioeconomic factors also play an important role in the decision-making process, as described in detail in this section.
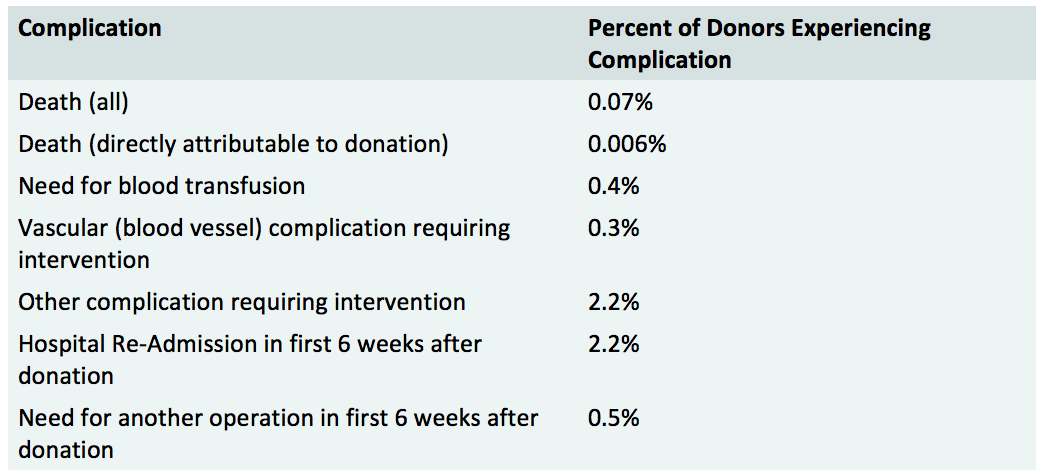
The following is a comprehensive list of complications that may occur surrounding the surgery to donate a kidney:
Kidney donors typically experience a 20 to 30 percent decrease in kidney function (as measured by the glomerular filtration rate) after donation. The remaining kidney compensates for the loss of one kidney, through a process called hyperfiltration. Other complications that may occur in the long-term following surgery to donate a kidney include:
Considering living donation can be scary and challenging for the potential donor.
On one hand, the potential donor may be worried about their potential recipient or may feel guilty about the health problems that person is experiencing. On the other hand, the potential donor will likely feel stress and concern related to the possibility of donating their organ, which requires them to undergo surgery themselves.
The good news is that most potential donors have similar questions and concerns. Dedicated donor teams – including transplant coordinators, physicians, social workers, and psychiatrists – are well-versed in helping potential donors answer these questions for themselves and cope with any issues that arise.
Some concerns expressed by many potential donors include:
Living kidney donors may be at risk for experiencing the following:
Many potential kidney donors have questions regarding the financial impact of becoming a donor. There will be both covered expenses (paid by the intended recipient's insurance) and non-covered expenses associated with evaluation and donation that potential donors need to consider carefully.
The insurance of the intended recipient of your kidney (Medicare or private health insurance) covers the testing needed to see whether or not you can be a donor (called the evaluation process) as well as the surgery and hospitalization needed for the kidney donation.
In general, some follow-up/post-operative care is covered, but not all. The extent of covered follow-up care will vary depending on your recipient's insurance.
In general, the following expenses are not covered by insurance, so should be considered "out-of-pocket" costs:
All donors are required to have health insurance in the event that any medical issues/diagnoses arise during the course of their evaluation to be a donor.
In this instance, the recipient's insurance does not cover the donor's medical expenses, so the potential donor must have health insurance in place to ensure that they will be covered in such a circumstance.
Kidney donation may also be considered a pre-existing condition. Although current law largely prohibits the denial of insurance based on pre-existing conditions, some insurance companies are still allowed to deny coverage for this reason. This is another reason why obtaining health insurance prior to donation is important.
In some cases, having been a kidney donor can impact the donor's ability to obtain both health insurance and life insurance. Therefore, it is highly recommended that people considering donation obtain these types of insurance prior to becoming a donor.
New York: there is a $ 10,000 organ donation tax deduction. Living donors can deduct up to $10,000 on their state income taxes for donation-related expenses such as travel, lodging, and lost wages. To learn more about tax deductions and credits for living donors, visit the National Kidney Foundation Web site.
The National Organ Transplantation Act of 1984 specifically prohibits the exchange of "valuable consideration" for a human organ ("It shall be unlawful for any person to knowingly acquire, receive, or otherwise transfer any human organ for valuable consideration for use in human transplantation").
Therefore, it is illegal to sell organs; if this occurs, it is punishable by fines, imprisonment, or both.
However, the payment of "the expenses of travel, housing, and lost wages incurred by the donor of a human organ in connection with the donation of the organ" is expressly permitted by section 301 of NOTA.
Learn more about the National Organ Transplantation Act (pdf).
Since the mid-to-late 1990's, advances in surgical techniques have dramatically improved the cosmetic result following living kidney donation.
Below, you can view pictures of scars from donors who have had the different types of surgical procedures to remove their kidney. Seeing this progression helps you to appreciate how much less invasive today's procedures are when compared to the open donor nephrectomy, and also demonstrates how these techniques have led to a significant reduction in the donor's recovery time.
The current standard of care at NewYork-Presbyterian/Weill Cornell, a pioneering center of this technique.

The way the donor surgery is currently performed at most centers that do not yet perform laparoendoscopic single site surgery.

The way the donor surgery was performed up until the mid- to late-1990's

In many ways, the benefits of kidney donation are personal and cannot be known by anyone other than the person that is donating or has donated.
Each donor's motivations may vary greatly and each donor has a unique experience as they go through the journey of donating their kidney, from the initial decision to be evaluated as a potential donor to years after the donation occurs.
The following information has been compiled from various research studies that have attempted to quantify the benefits and/or quality of life of kidney donors as a result of the donation.
To summarize the key findings:
In addition, the intense screening process that donors must undergo has helped some potential donors receive diagnoses that may benefit from early intervention, such as cancer.
At times, screening has led to early detection of the potential donor's own medical issues such as kidney disease, high blood pressure, diabetes, and cardiac disease, which can benefit from early diagnosis and intervention.