The vulva includes the inner and outer lips of the vagina, clitoris, vaginal opening, and vaginal glands. A rare form of cancer, vulvar cancer occurs when cancerous cells develop in any part of the vulva. Vulvar cancer is very curable when detected at an early stage.
At Weill Cornell Medicine, our expert gynecologic oncologists care for vulvar cancer patients compassionately. Our physicians utilize novel treatment techniques, such as sentinel groin node biopsy to maximize the chance for cure with an emphasis on quality of life. Our patients benefit from easy access to their attending physicians through video visits, e-message, flexible scheduling, and collaborative care with a wide range of specialists.
Women who have contracted the human papillomavirus (HPV), use tobacco, have the human immunodeficiency virus (HIV), or have other genital cancers are at a higher risk for developing vulvar cancer.
While the HPV vaccine is approved for the prevention of cervical cancer and precancers, it protects against the types of HPV virus that can also cause vulvar cancer. Optimally, the HPV vaccine is given to preteens prior to exposure to the virus. In addition, quitting tobacco use and using condoms may help prevent vulvar cancer.
Precancerous conditions may be detected on the vulva at the time of a routine annual gynecology visit prior to the onset of symptoms. Self–examination with the assistance of a mirror may also be helpful in the early detection of vulvar abnormalities. Any new findings, particularly raised, whitish, hyperpigmented and/or painful ulcers should be immediately brought to your physician’s attention.
The most common signs of vulvar cancer include:
Your physician will first conduct a physical and pelvic exam. A biopsy is the best way to confirm the diagnosis, so a small sample of cells is removed from the vulva and examined under a microscope.
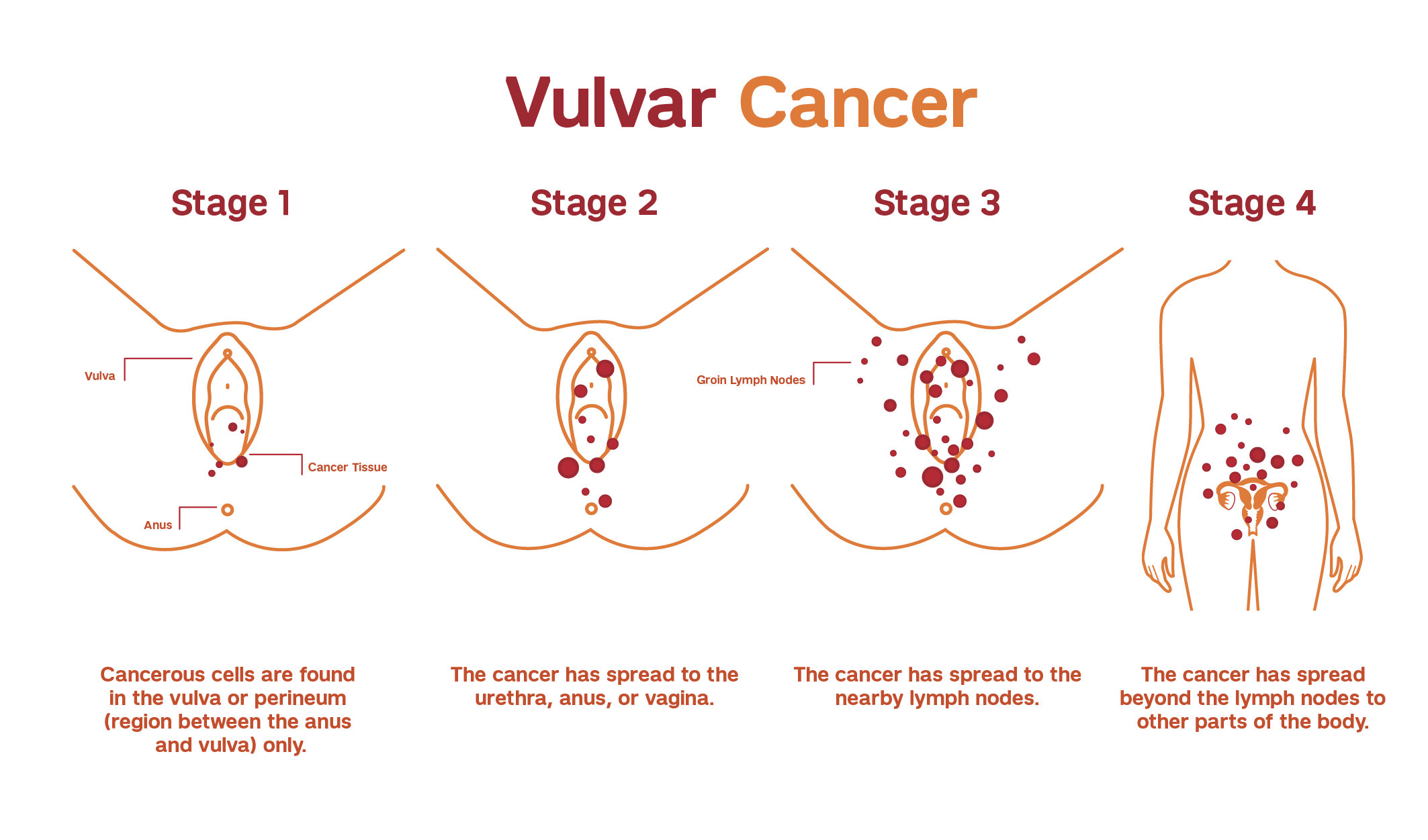
If vulvar cancer is confirmed, it is critical to determine if and where the cancer has spread and the extent of disease. Our team of expert gynecologic oncologists carefully evaluate each patient to determine the stage of vulvar cancer and develop a personalized treatment plan.
Imaging tests may include a CT, MRI, or PET scan.
Our team of gynecologic oncologists personalize treatment depending on many factors, including vulvar cancer stage and the potential for complications involving bladder, rectal, and sexual function.
Individual treatment plans may include a combination of surgery, radiation therapy, chemotherapy, immunotherapy, and other treatment options. Our physicians work closely with patients to minimize side effects and promote greater comfort throughout treatment.
Treatment for early-stage tumors typically involves surgery, while more advanced stages are typically treated with a combination of therapies, including preoperative radiation and chemotherapy to limit the extent of surgery.
If precancerous cells are detected, our gynecologic oncologists can remove them surgically or by laser ablation. These treatments are limited, removing only the precancerous parts of the vulva. Precancerous cells can also be removed with topical therapy (a cream or ointment that is put directly on the precancer).
There are several surgical options to treat vulvar cancer, all of which include removing cancerous tissue (excision). A gynecologic oncologist will evaluate your specific condition and present the most appropriate options.
If the cancer has spread to a certain point, your physician may recommend:
Sentinel lymph node biopsy is a procedure which identifies and removes the node or group of nodes to which the vulvar cancer is likely to spread first. This procedure helps physicians determine the extent of disease, as well as prevent the need for a full groin lymph node dissection.
Our gynecologic oncologists work closely with expert radiation oncologists at Weill Cornell Medicine to treat appropriate vulvar cancer patients with radiation therapy.
Chemotherapy is the use of drugs to kill cancerous cells. To limit side effects and damage to healthy cells, vulvar cancer patients are usually given chemotherapy in cycles with several rest periods. Our patients benefit from Weill Cornell Medicine's state-of-the-art chemotherapy treatment center, which provides unique support and resources.
Immunotherapy is the use of medications to stimulate your immune system to recognize and destroy cancer cells more effectively. Your physician determines the best immunotherapy medications and timing for taking them.
With care from a highly trained gynecologic oncologist, immunotherapy can be an integral part of your vulvar cancer treatment.
The gynecologic oncologists at Weill Cornell Medicine collaborate with other specialists and researchers within the cancer center to offer unparalleled interdisciplinary care at our top-ranked hospital.
Weill Cornell Medicine patients have access to specialists in gynecology, surgical oncology, medical oncology, pathology, radiation oncology, genetics, nutrition, social work, and reproductive medicine. In addition, our patients benefit from collaborative care with:
Our gynecologic oncologists and physician assistants work closely with patients to promote wellness during and after treatment – with the goal of helping you return to the full breadth of functional living you enjoyed before the diagnosis. Our team provides frequent follow-up care and monitoring for recurrence.
In addition, we will connect you with support groups, services, and resources to live as fully as possible.