Vaginal cancer is the rarest of gynecologic cancers. It begins in the vagina, the muscular tube that connects the outer genitalia to the uterus (also called the “birth canal”).
Vaginal cancer patients find comfort in our personalized, holistic, and warm approach to care at Weill Cornell Medicine. In addition to access to experts at a leading academic medical center, our patients also benefit from greater access to their attending physician, video visits, e-message, flexible scheduling, and collaborative care with a wide range of specialists.
Women who are over 50 years old, took diethylstilbestrol (DES), use tobacco, or have the human papillomavirus (HPV) have a greater risk of developing vaginal cancer.
The HPV vaccine protects against the HPV virus that can cause vaginal cancer. Typically, the HPV vaccine is given to preteens. In addition, quitting tobacco use and using condoms can help prevent vaginal cancer.
There is no recommended screen for vaginal cancer. Precancerous cells of the vagina can at times be detected by Pap smears performed for cervical cancer screening.
The most common signs for vaginal cancer include:
Your physician will first conduct a physical and pelvic exam. A biopsy is the best way to confirm the diagnosis, so a small sample of cells is removed from the vaginal wall and examined under a microscope.
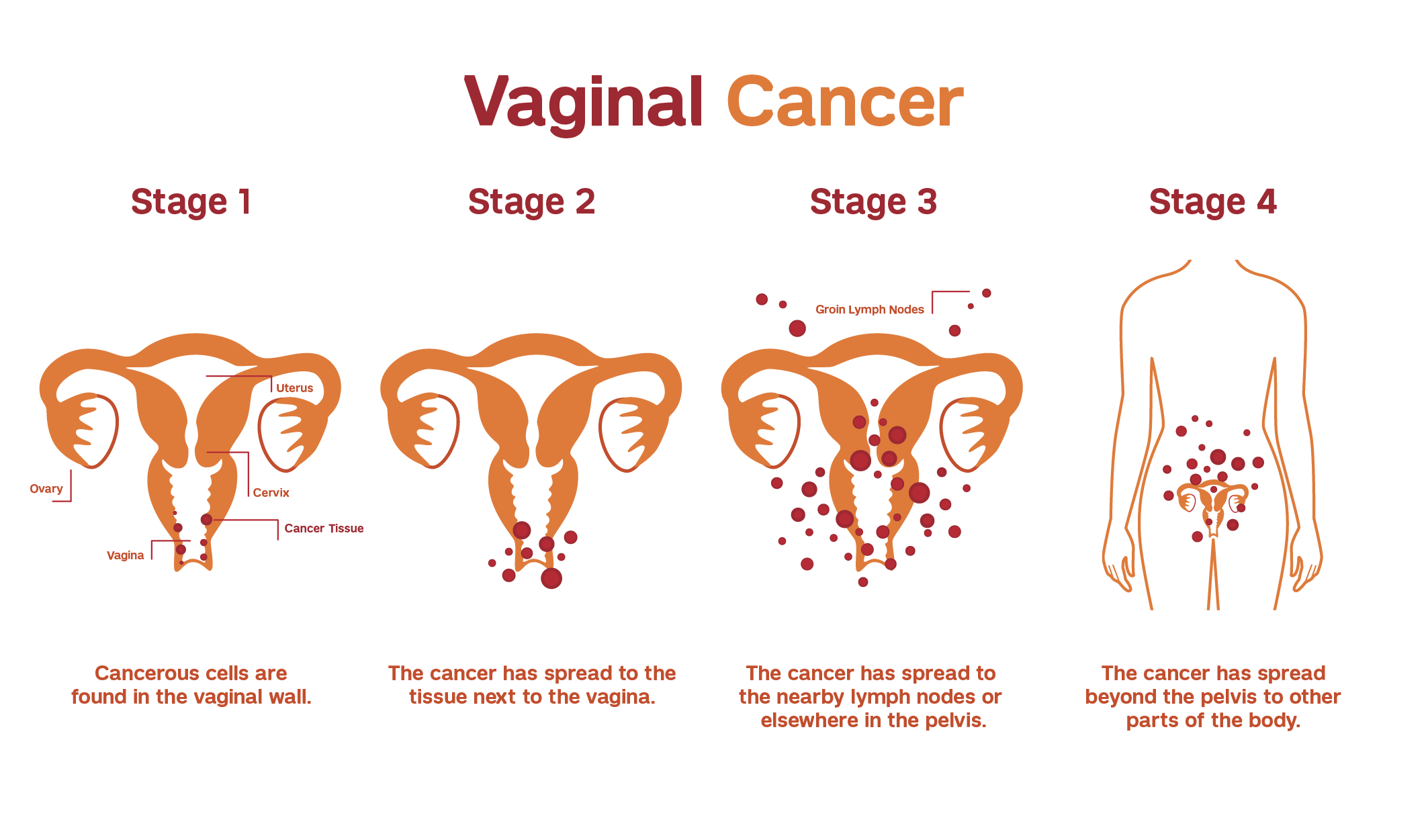
If vaginal cancer is confirmed, it is critical to determine where the cancer is and the extent of disease. Our team of expert gynecologic oncologists carefully evaluate each patient to determine the stage of vaginal cancer and develop a personalized treatment plan.
Imaging tests may include a CT, MRI, or PET scan.
Our team of gynecologic oncologists personalize treatment depending on many factors, including the extent of disease.
Individual treatment plans may include a combination of surgery, radiation therapy, chemotherapy, immunotherapy, and other treatment options. Our physicians work closely with patients to minimize side effects and promote greater comfort throughout treatment.
If precancerous cells are detected, our gynecologic oncologists can surgically remove them with laser ablation. Precancerous cells can also be treated with topical therapy (a cream or ointment that is put directly on the cancer).
There are several surgical options to treat vaginal cancer, all of which include removing cancerous tissue (excision). A gynecologic oncologist will evaluate your specific condition and present the most appropriate options. Your physician may recommend:
Sentinel lymph node biopsy is a procedure in which the sentinel lymph node is removed and biopsied for cancer cells. Cancer typically spreads to these nodes first. This procedure helps physicians determine the extent of disease, as well as prevent the need for a full pelvic lymph node dissection.
Since several important organs are located in close proximity to the vagina, it is important to seek a highly trained surgeon who specializes in gynecologic cancers.
Our gynecologic oncologists work closely with expert radiation oncologists at Weill Cornell Medicine to treat appropriate vaginal cancer patients with radiation therapy.
Chemotherapy is the use of drugs to kill cancerous cells. To limit side effects and damage to healthy cells, vaginal cancer patients are usually given chemotherapy in cycles with several rest periods.
Most women receive intravenous chemotherapy in combination with radiation to increase the effectiveness of radiation. Our expert gynecologic oncologists determine the most effective combination of therapies for each patient depending on a variety of factors.
Our patients benefit from Weill Cornell Medicine's state-of-the-art chemotherapy treatment center, which provides unique support and resources.
Immunotherapy is the use of medications to stimulate your immune system to recognize and destroy cancer cells more effectively. Your physician determines the best immunotherapy medications and timing for taking them.
With care from a highly trained gynecologic oncologist, immunotherapy can be an integral part of your vaginal cancer treatment.
Our gynecologic oncologists work closely with the expert reproductive medicine specialists at Weill Cornell Medicine to offer vaginal cancer patients options to preserve fertility, including egg or embryo freezing.
The gynecologic oncologists at Weill Cornell Medicine collaborate with other specialists and researchers within the cancer center to offer unparalleled interdisciplinary care at our top-ranked hospital.
Weill Cornell Medicine patients have access to specialists in gynecology, surgical oncology, medical oncology, pathology, radiation oncology, genetics, nutrition, social work, and reproductive medicine. In addition, our patients benefit from collaborative care with:
Our gynecologic oncologists and physician assistants work closely with patients to promote wellness during and after treatment – with the goal of helping you return to the full breadth of functional living you enjoyed before the diagnosis. Our team provides frequent follow-up care and monitoring for recurrence.
In addition, we will connect you with support groups, services, and resources to live as fully as possible.