Pelvic organ prolapse (POP) results when one or more of the pelvic organs drops into the vaginal canal. The pelvic floor consists of the muscles, nerves and connective tissue that surround the uterus, vagina, bladder and rectum, providing support and helping these organs function properly. When these support structures become weakened, the pelvic organs can begin to fall out of their normal position. The movement of these organs, or prolapse, may make it more difficult for these organs to function normally.
Other names for pelvic organ prolapse include cystocele or "fallen bladder" (bladder prolapse), rectocele and "dropped uterus" (uterine prolapse).
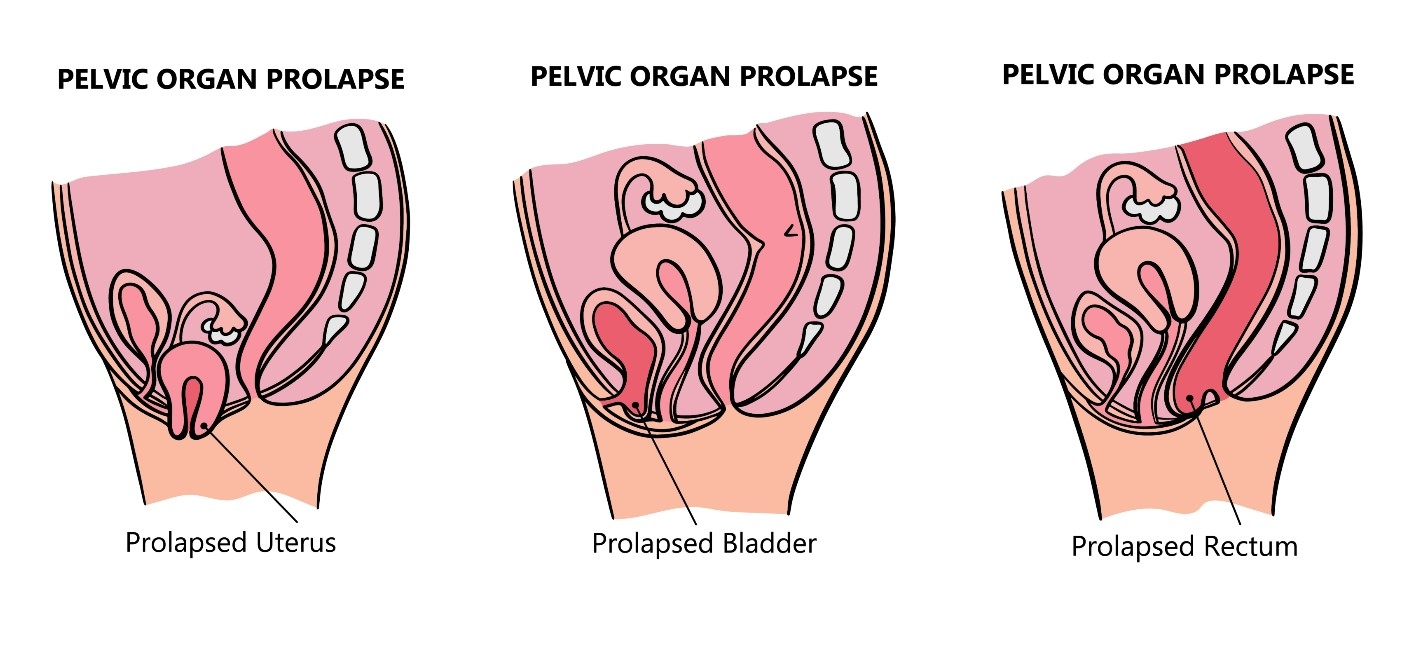
There are different types of pelvic organ prolapse:
- Cystocele prolapse: the bladder bulges or pushes into the vagina
- Rectocele prolapse: the rectum tissues bulge or pushes into the vagina
- Enterocele prolapse: the small intestine bulges or pushes into the vagina
- Uterine prolapse: the uterus drops into the vaginal canal
- Vaginal prolapse: the top of the vagina drops into the vaginal canal
Pelvic Organ Prolapse Symptoms
Perhaps the most obvious symptom of pelvic organ prolapse is a noticeable bulge protruding from the opening of the vagina.
Additional symptoms of POP include:
- Feelings of pelvic pressure or discomfort
- Perception of something falling out
- Difficulty emptying the bladder
- Difficulty emptying the rectum
Causes and Risk Factors for Pelvic Organ Prolapse
Despite the high prevalence of this disorder, the exact cause of pelvic organ prolapse is unknown. With that said, there are risk factors that increase the chances of developing POP.
Risk factors may include:
- Pregnancy
- Vaginal delivery (in particular, difficult or prolonged deliveries)
- Bowel dysfunction, including constipation or chronic straining
- Chronic coughing
- Genetic connective tissue weakness
- Age
- Family history of prolapse
- Obesity
Prevention Strategies for Pelvic Organ Prolapse
While the precise cause pelvic organ prolapse is unknown, some ways to help prevent or manage side effect include:
- Treat constipation or chronic coughing
- Quit smoking
- Maintain a healthy weight
- Pelvic floor exercises to strengthen the muscles
Treatment Options for Pelvic Organ Prolapse
Pelvic organ prolapse is diagnosed by physical exam in which the physician evaluates the anterior vaginal wall, posterior vaginal wall, top of the vagina and uterus, inspecting for signs of pelvic organ prolapse. The prolapse is then carefully measured with the patient straining. It is important for the physician to carefully measure all aspects of pelvic floor support before suggesting a treatment plan.
POP can be treated with a variety of non-surgical and surgical options, depending on the severity of the condition.
Non-surgical treatment options:
- Kegel exercises: Exercises best used for mild cases of prolapse to strengthen the muscles of the pelvis. As with any exercise program, Kegel exercises must be done correctly and regularly to work.
- Pelvic floor therapy: Consists of visits to a physical therapist with specialized training in pelvic floor disorders. These specialized physical therapists utilize various techniques, depending on the condition they are treating. With pelvic organ prolapse, the goal of pelvic floor therapy is to strengthen the pelvic floor to support the vagina and pelvic organs.Treatment options commonly used in pelvic floor therapy are:
- Biofeedback: An intravaginal device to train pelvic floor muscles to contract and relax properly.
- Functional electrical stimulation: A device that can be used intravaginally or externally, delivering a gentle electrical current to activate muscles in the pelvis.
- Vaginal pessary: A removable, diaphragm-like device worn within the vagina to support the bladder or other organs that are prolapsing through the vagina. A vaginal pessary may also be used to decrease stress urinary incontinence. Pessaries come in a variety of types and sizes. Pessary fitting may require two or more office visits to select the proper type and size of pessary that will work for you.
Surgical treatment options:
Vaginal "Native-Tissue" Prolapse Repair:
- Anterior Colporrhaphy: A vaginal surgery using the patients' existing tissue to reduce the bulging and lift the bladder up.
- Posterior Colporrhaphy: A vaginal surgery using the patient's existing tissue to reduce the bulging and support the wall between the rectum and vagina.
- Perineorrhaphy: The surgical repair of a weakened perineum (the area between the vaginal opening and the anus).
- Vaginal Vault Suspension/Uterine suspension: The suspension of the top (or "apex") of the vagina to a ligament in the pelvis, usually either the sacrospinous ligament or the uterosacral ligaments.
- Hysterectomy (removal of the uterus): Hysterectomy is often performed as the first step of a prolapse repair, because doing so often allows for a better suspension of the vagina to the surrounding support structures.
- Colpocleisis: Involves closure of the vagina to fix and prevent recurrence of prolapse. This is not an option for patients who have penetrative sexual activity.
Robotic or Laparoscopic Prolapse Repairs:
- Robotic or Laparoscopic Sacrocolpopexy: Involves fashioning a 'custom-made' Y-shaped mesh that will reconstruct the entire support system of the pelvic organs through attachment to a ligament near the backbone in the pelvis. Described as the "gold-standard" prolapse repair and is usually performed laparoscopically or robotically for less discomfort during the healing process.
- Robotic or Laparoscopic Hysterectomy (removal of the uterus): Hysterectomy is often performed as the first step of a prolapse repair, because doing so often allows for a better suspension of the vagina to the surrounding support structures.
- Other surgical options can include either synthetic mesh or biodegradable mesh to help support the prolapsed organs. The use of this mesh provides stronger support than using a patient’s own tissue.
Would you like an appointment?
To request an appointment, please call our office at (646) 962-7400 or schedule an appointment with one of our providers online below. Our phone staff are available to help you Monday-Friday, from 9AM-5PM (EST).
Meet our expert providers who specialize in treating Pelvic Organ Prolapse: