Overactive bladder (OAB) is a condition where the bladder improperly stores urine which leads to symptoms of daytime and nighttime urinary frequency and urinary urgency.
OAB can be subdivided into "wet" or "dry.” Wet OAB, in which urinary urgency leads to leakage of urine, is also known as “urinary incontinence”, and it affects an estimated 10-15% of women in the United States. Dry OAB does not lead to leakage of urine and affects an estimated 30% of women in the United States.
Female Overactive Bladder Symptoms
There are three common symptoms of overactive bladder:
- Urinary urgency: A sudden and intense desire to urinate, which may occur with or without leakage of urine (wet vs. dry). The symptom of urinary urgency can be triggered by specific situations such as hearing running water, touching running water or getting close to a bathroom, or returning home. With wet OAB, a person may be unable to stop the urine from leaking out before reaching the toilet.
- Daytime urinary frequency: Increased need to urinate during the day. Many patients with overactive bladder must urinate every 1-2 hours during the day. For some patients with overactive bladder, the sensation to urinate never goes away.
- Nocturia (nighttime urination): The need to urinate that awakes someone from sleep. The patient typically wakes up to urinate and then will go back to sleep after. For some patients, this occurs multiple times per night which leads to significant sleep disruptions.
It is important to have a medical evaluation of the symptoms of overactive bladder because they can also be related to other conditions such as urinary tract infections, pelvic organ prolapse, or urinary retention.
Causes and Risk Factors for Female Overactive Bladder
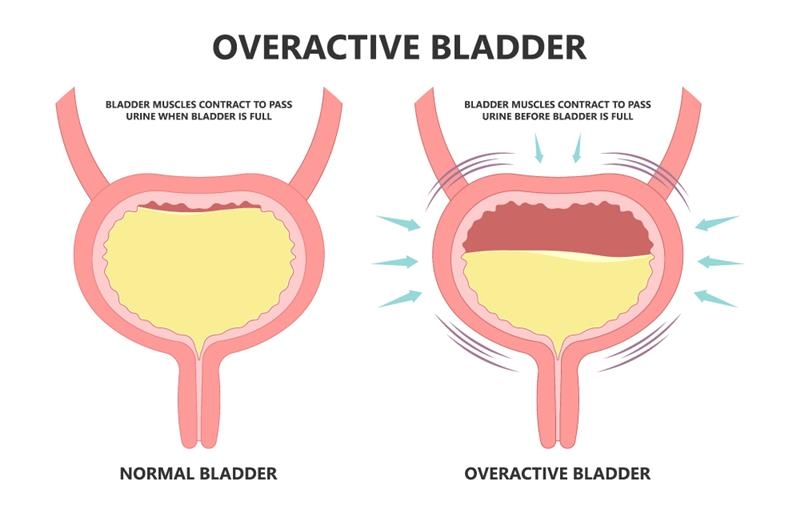
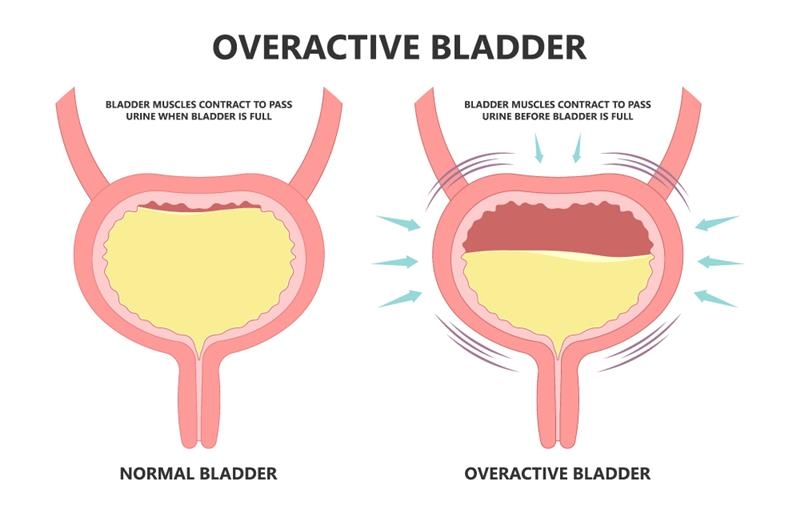
Overactive bladder can be caused by an involuntary bladder muscle contraction as the bladder fills with urine. It can also be an increased sensory response from the bladder in which your body alerts your body about the need to urinate without having much urine inside the bladder.
Risk factors for overactive bladder include:
- Older age
- Menopause
- Obesity
- Presence of neurological conditions (i.e., stroke, Parkinson's disease, multiple sclerosis or diabetes)
Medications and diet can sometimes contribute to overactive bladder symptoms as well. For example, smoking and alcohol can irritate the bladder and contribute to increased need to urinate and urinary urgency. Medications that pull fluid out of your body or cause diuresis can also contribute to overactive bladder medicines. It is important to discuss with your doctor if you start to experience overactive bladder after starting a new medication.
Prevention Strategies for Female Overactive Bladder
Overactive bladder is not always preventable. If there is an underlying cause such as obesity, diet, or medication, then there are ways to manage this.
Ways to manage OAB include:
- Dietary modifications, such as managing fluid intake or limiting bladder irritants (i.e., soda, alcohol, sugar, teas, etc.)
- Bladder retraining
- Improving toileting habits
- Not smoking
- Managing a healthy weight through diet and physical exercise
- Pelvic floor muscle strengthening and exercises
Treatment Options for Female Overactive Bladder
Both non-surgical and surgical treatment options are available for treating OAB.
Non-surgical treatment options:
- Kegel exercises: Used to strengthen the muscles of the pelvic floor. These exercises control stress urinary incontinence, urge urinary incontinence, overactive bladder and fecal incontinence and may be used to slow the progression of vaginal prolapse. Kegel exercises must be done correctly and regularly.
- Pelvic floor therapy: Consists of visits to a physical therapist (PT) with specialized training in pelvic floor disorders. These PTs use a combination of techniques to help strength and control the pelvic floor muscles depending on the type of condition they are treating.
- Behavioral modification: Consists of education on diet, fluid intake and other lifestyle changes to manage various bothersome symptoms.
- Bladder training: Consists of changing lifestyle habits that may be worsening OAB and learning to use the pelvic floor muscles to suppress OAB symptoms, including urinary urgency, nocturia and urge urinary incontinence.
- Biofeedback: Uses special equipment to visually guide the patient on how to train pelvic floor muscles to contract and relax properly. Sensors can be placed on the skin to measure the muscle activity.
- Functional electrical stimulation: Utilizes a device that can be used intravaginally or externally, delivering a gentle electrical current to activate or relax the nerves and muscles in the pelvis.
- Overactive bladder medications: These treat overactive bladder by relaxing the bladder muscle to help the bladder store more urine and suppress urges to urinate. Some historically prescribed medications may cause dry mouth, dry eyes, blurred vision, urinary retention, constipation, dizziness or drowsiness; however, the newer class of medications are much safer with most patients reporting no side effects
- Percutaneous Tibial Nerve Stimulation: An FDA-approved treatment for OAB where an acupuncture needle is placed next to the tibial nerve in the ankle and connected to an electrical stimulator. This device sends low voltage electrical currents to the tibial nerve for 30 minutes. Treatments occur 1 time per week for 10-12 weeks.
Surgical treatment options:
- Sacral nerve modulation: An FDA-approved treatment for urinary urgency, frequency, urge incontinence and retention. This treatment uses a small device that is implanted under the skin of one of the upper buttocks. It works by gently stimulating the sacral nerves to help the bladder function more normally.
- Chemodenervation of the bladder (botulinum toxin type A): This consists of injecting botulinum toxin A (commonly known as “botox”) directly inside of the bladder with a cystoscopy. This can be done in the office or in the operating room based on patient preferences. It can be very effective in patients with overactive bladder or urge urinary incontinence who are not responsive to medications.
- Implantable Tibial Nerve Stimulators: E-Coin is an FDA-approved treatment for overactive bladder. A small coin-shaped device is implanted under the skin of one ankle. The device sends electrical stimulation to the tibial nerve to help the bladder function properly.
Would you like an appointment?
To request an appointment, please call our office at (646) 962-7400 or schedule an appointment with one of our providers online below. Our phone staff are available to help you Monday-Friday, from 9AM-5PM (EST).
Meet our expert providers who specialize in treating Female Overactive Bladder: