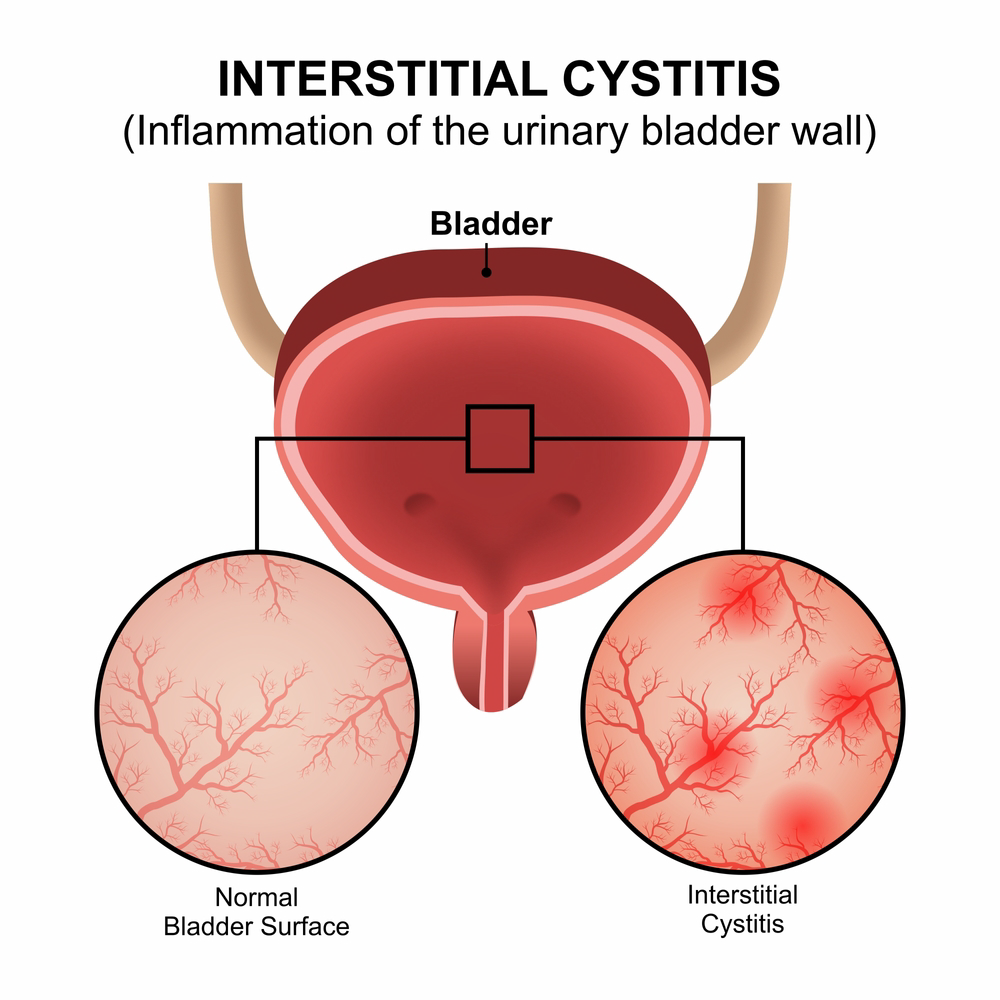
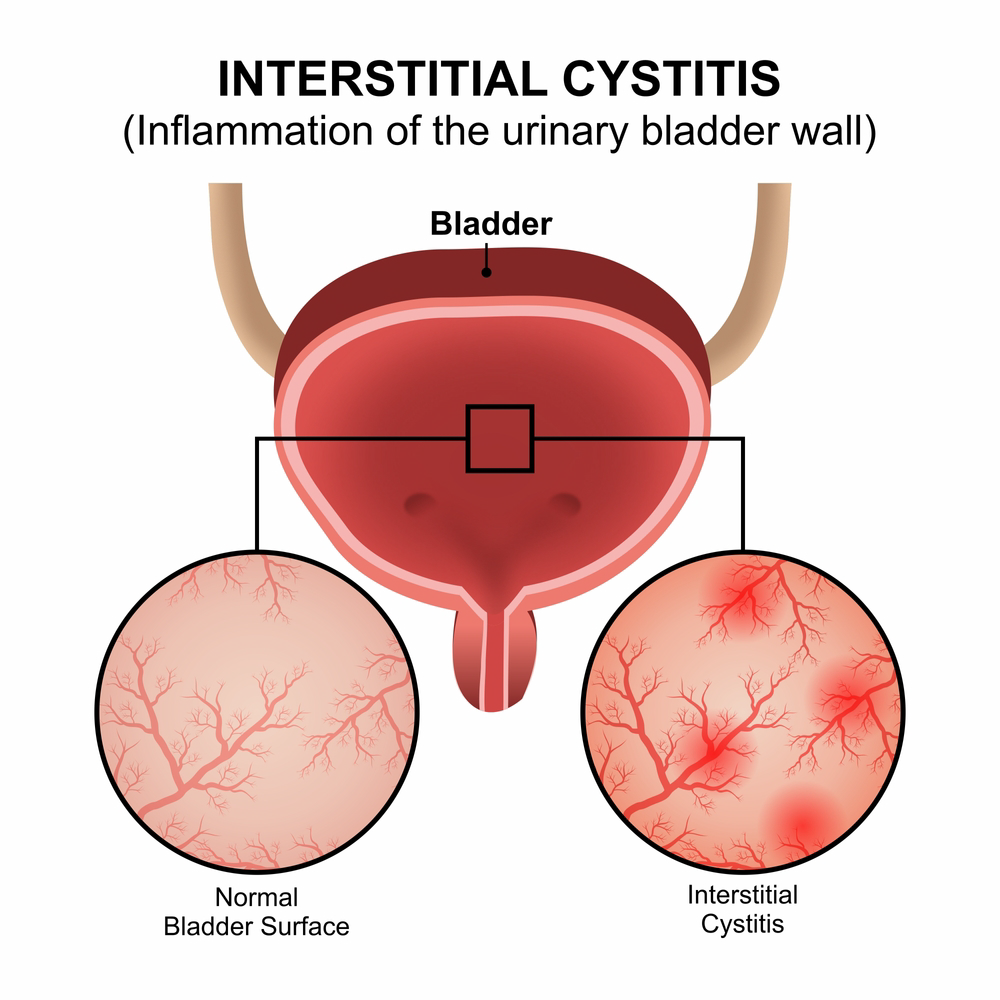
Interstitial cystitis (IC), also known as painful bladder syndrome (PBS), is a chronic condition that causes chronic bladder or urethral pain. It is a diagnosis of exclusion meaning it is not caused by another underlying condition such as a urinary tract infection or bladder or kidney stone.
Interstitial Cystitis Symptoms
Common symptoms of interstitial cystitis include:
- Pain in bladder or urethra that is worse with filling and relieved with emptying the bladder
- Urinary urgency
- Urinary frequency
- Nocturia (being awakened by the urge to urinate more than once per night)
The intensity of these symptoms may range from mild to debilitating. Some foods and beverages, as well as tobacco, tend to make the symptoms worse. It is recommended that patients with interstitial cystitis follow an IC diet which consists of food with low acidity. Women suffering from PBS/IC may also suffer from additional pain syndromes such as, irritable bowel syndrome, fibromyalgia, migraines, endometriosis, and vulvodynia.
Causes and Risk Factors for Interstitial Cystitis
The exact cause of IC is unknown. However, we do have ways to treat these symptoms.
Management Strategies for Interstitial Cystitis
While we don’t know the exact causes of interstitial cystitis, some ways to help prevent or manage symptoms include:
- Dietary modifications, including avoiding triggers (coffee, alcohol, teas, soda, spicy food, acidic food, etc.)
- Reduce stress
- Quit smoking
- Pelvic floor relaxation exercises
- Manage other chronic conditions
Treatment Options for Interstitial Cystitis
While there is no test for the diagnosis of interstitial cystitis, sometimes testing is done to rule out other possible causes of the symptoms such as bladder cancer, urinary stones, urinary tract infections or other gynecological problems.
While there is no cure for IC, there are several management options available. Most patients are able to find a treatment regimen that works for them and controls their symptoms. However, sometimes finding the combination of options that will provide relief often requires diligence and patience.
Non-surgical treatments options:
- Bladder diet: Avoiding food and beverages that irritate the bladder and intensify urinary symptoms. A "bladder elimination diet" is a method to determine which foods and beverages make your symptoms worse.
- Pelvic floor therapy: Consists of visits to a physical therapist with specialized training in pelvic floor disorders. These specialized physical therapists utilize a combination of various techniques, listed below, depending on the type of urogynecological condition they are treating. Typically, patients with interstitial cystitis need to focus on relaxation techniques of the pelvic floor muscles.
- Joint and tissue mobilization: Therapy involving gentle manipulation to help calm the muscles and nerves of the pelvis.
- Bladder instillations: Repeated instillations of lidocaine, heparin and other substances into the bladder to decrease bladder pain. The mixture is instilled through a small catheter inserted into the urethra two times per week until the desired results are achieved.
Surgical treatment options:
- Cystoscopy with fulguration: A minimally invasive procedure which involves burning ulcers associated with IC
- Cystoscopy with hydrodistention: A minimally invasive procedure which involves distending the bladder under anesthesia.
- Sacral nerve modulation: Interstitial cystitis is an off-label use for Sacral nerve modulation. This is a small device that is implanted under the skin of one of the upper buttocks. It works by gently stimulating the sacral nerves to help the bladder function more normally.
- Cystoscopy with Botox injections: Minimally invasive procedure as an off-label use for interstitial cystitis. Involves injecting Botox into the bladder muscle.
Would you like an appointment?
To request an appointment, please call our office at (646) 962-7400 or schedule an appointment with one of our providers online below. Our phone staff are available to help you Monday-Friday, from 9AM-5PM (EST).
Meet our expert providers who specialize in treating Interstitial Cystitis: