To help you better understand the process of organ donation and transplantation, we have compiled the following list of common terms and procedures.
ABO incompatible transplant — In some cases, it is possible to transplant a kidney from a blood-type incompatible donor into a patient who needs a kidney. In these cases, extra therapy is required before the transplant in order to overcome the incompatibility. These therapies include rituximab, intravenous immune globulin, and plasmapheresis, a procedure that removes antibodies from the blood.
Access — Patients with kidney failure require an access site to receive dialysis through since the volume of blood that needs to be cleaned is high. Types of dialysis access include catheters, fistulas, and grafts.
Adherence - Also called "compliance", this is the act of following instructions, such as attending dialysis sessions and taking medications as prescribed. Adherence is a very important component of transplantation since loss of the transplant may occur when patients are not adherent to their medication and follow-up schedules.
Allocation — This is the process used by the United Network for Organ Sharing to distribute organs for transplant to the most suitable recipient, based on waiting time and matching of the donor and recipient.
Allograft — Another term for a transplanted organ. Sometimes referred to as "graft". For example, a kidney transplant may be called a kidney allograft or kidney graft.
Altruistic donor — A person who wishes to be a living kidney donor although they do not have a specific person in mind to donate to. Altruistic donors are key to the success of donor chain transplants since their participation enables many transplants to occur. Altruistic donors are also known as "non-directed" or "Good Samaritan" donors. View the video for "Altruistic Kidney Donations Save Lives" on YouTube.
Anti-rejection medication — Also known as immunosuppressants, these are the medications that transplant patients must take for as long as their transplant continues to function in order to lower the risk that the immune system will try to reject the transplanted organ.
Antibody — An antibody is made by the immune system in response to a foreign intruder such as an infection or a transplanted organ. The antibody locks onto the cells of the invader, which signals the immune system to destroy the cell.
Antigen — These are proteins present on the surface of cells that enable the immune system to tell that the cell is an invader. In response to the foreign antigens, the immune system then creates antibodies which then latch on to the antigen proteins and signal the immune system to destroy that cell.
Biopsy — A biopsy is a procedure performed so that the transplanted organ can be examined under a microscope. Currently, biopsies are the gold standard for diagnosing rejection of the transplant organ. In addition, biopsies can provide other important information about the function of the transplant, such as infection or recurrence of kidney disease. During a biopsy, a needle is introduced into the transplanted organ under local anesthesia.
Bladder — The bladder holds urine made by the kidneys until it is ready to be released from the body. During a kidney transplant, the new kidney is attached to the bladder using the ureter (tube that carries urine from the kidney to the bladder) of the donor. In order for the bladder to heal from the surgery, a Foley catheter is placed in the bladder so that the urine produced by the new kidney can be continuously drained from the body while the bladder heals.
Blood pressure — High blood pressure is a leading cause of kidney disease since the increased pressure can damage the kidney over time. After transplant, it is important that the blood pressure is neither too high nor too low in order to ensure the best outcomes. Control of blood pressure after transplant is also very important to prevent damage to the transplanted kidney.
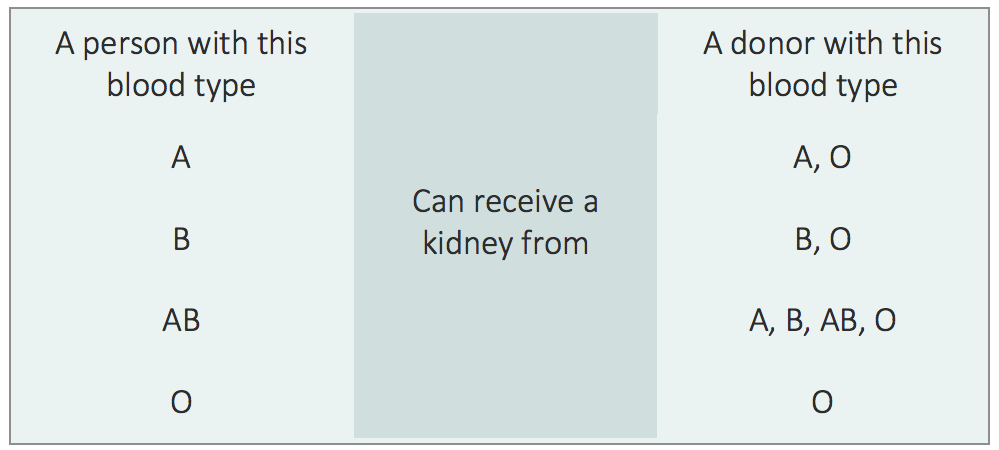
Blood Type — Each person has a specific blood type, A, B, AB, or O. Blood type is very important for both blood transfusions and transplantation because incompatibility can cause a reaction that could lead to loss of the transplant. The table below shows transplant blood type compatibility.
Brain death — The majority of deceased organ donors are declared brain dead. Although their heart and lungs may be temporarily functioning due to artificial support systems (such as a ventilator), the person has no brain activity and therefore no possibility of recovery.
Cadaveric donor — An older term for a person who has donated their organs upon death. The term now used is “deceased donor”.
Chronic kidney disease (CKD) — All patients who need a kidney transplant have chronic kidney disease which has progressed to the point of needing dialysis and/or a kidney transplant.
Coercion — Coercion is when a donor feels compelled to donate out of fear, guilt, pressure or other emotion. Other words for coercion include "arm-twisting", force, compulsion, constraint, duress, and pressure.
Potential donors should realize that their health information is protected by the living donor team and is not shared with the potential recipient or the healthcare professionals caring for your potential recipient. If a potential donor feels coerced into donating, the living donor team will be able to provide that potential donor with a "way out" based on medical reasons that will not be disclosed to the potential recipient.
Cold ischemia time — This is the amount of time that an organ is out of the body, in between being removed from the donor, and being placed into the transplant recipient. For deceased donor kidney transplantation, the cold ischemia time often exceeds 24 hours; in general, kidneys can be out of the body for up to 48 hours. The longer the cold ischemia time, the longer the kidney may take to "wake-up" and begin to function after being transplanted.
Compliance — Also called "adherence", this is the act of following instructions, such as attending dialysis sessions and taking medications as prescribed. Compliance is a very important component of transplantation since loss of the transplant may occur when patients are not compliant with their medication and follow-up schedules.
Crossmatch — A crossmatch is a test performed to see if a donor and recipient are compatible. The blood of the donor and recipient are mixed, and if there is a reaction, it is called a positive crossmatch. This reaction is caused by antibodies that the recipient has against the donor's antigens (described above). Depending on the severity of the positive crossmatch, it may indicate that the transplant should not go forward because the risk of rejection is too high.
Deceased donor — A term that has replaced ‘cadaveric’ donor - a person who has donated their organs upon death.
Delayed graft function (DGF) — This is a term for when the transplanted kidney does not "wake-up" and function right away after a transplant. A patient with delayed graft function will continue to need dialysis for a short period of time (usually a few days to several weeks) until the kidney wakes up.
Diabetes — A condition where the body cannot effectively use glucose (sugar) to fuel the body. Normally, insulin (a hormone made by the pancreas) acts as a key that allows glucose to enter into cells, where it is used as fuel (energy). In type 1 diabetes mellitus, the immune system attacks and destroys the pancreas (an organ that makes insulin), leading to requirement for insulin injections to survive. In type 2 diabetes, the body usually still makes insulin, but the insulin does not work effectively to allow glucose to enter the cells. Some patients with type 2 diabetes take pills to manage their diabetes, but sometimes will also require insulin injections.
Dialysis — A procedure used in patients with end stage renal disease to clean the body of toxins and extra fluid that the kidneys would normally get rid of. There are two kinds of dialysis — hemodialysis and peritoneal dialysis (see below for definitions).
Donation after cardiac death (DCD) — A deceased organ donor whose life support is removed in the operating room prior to organ donation. Often, organs from DCD donors take longer to "wake-up" and begin to function after transplantation.
Donation — The process of giving the gift of life by choosing to give your organ(s) for transplantation.
Donor — A person who chooses to donate their organ(s) for transplantation.
Donor chain - A chain of kidney transplants that occurs through a registry of incompatible donor and recipient pairs. By entering a registry, people who have a blood type or crossmatch incompatible donor can exchange donors with other incompatible pairs.
Donor Specific Antibody (DSA) — A lab test that measures the amount of antibodies that a transplant candidate has against their potential donor(s). High levels of DSA may prevent transplantation because the risk of rejection may be too high.
End-stage renal disease (ESRD) — Occurs when a patient has a chronic kidney disease that has progressed to the point that the kidneys no longer function and the patient requires dialysis or a kidney transplant to live.
Estimated Post-Transplant Survival (EPTS) Score — This is a calculated score that is used to estimate how long a kidney transplant candidate is expected to need a functioning kidney. It uses four factors, including age, diabetes, history of a prior transplant, and time on dialysis (if applicable). Patients with a low EPTS score (meaning they are young and will need a kidney for a long time) are matched with kidneys with a low KDPI score (meaning the kidney is expected to last longer). Read more about EPTS here.
Etiology — Another word for cause. For example, we like to know the etiology, or cause, of your kidney disease prior to transplantation. This is important because there are diseases that can recur in a transplant kidney that may affect how we manage you and your medications at the time of kidney transplantation. Learn more about the causes of kidney failure below.
Expanded criteria donor (ECD) — This is terminology that was used prior to 2014 used to describe a deceased donor who was age 60 years or older, or age 50 — 59 who had at least 2 of the following 3 conditions: high blood pressure, death from a stroke, and/or kidney impairment at the time of donation. Since the new kidney allocation system went into effect in late 2014, donor risk is quantified by the Kidney Donor Profile Index (KDPI) score, which is used to estimate the longevity of the transplanted organ. Kidneys with a KDPI score above 85 percent are considered similar to ECD kidneys.
No items for this section.
Glomerular filtration rate (GFR) — This is a measure of your kidney function. A GFR above 90 is generally considered normal, while a GFR less than 60 means that a person has kidney disease. Once the GFR falls to 20 or less, a person can be listed for a kidney transplant. Patients generally need dialysis once the GFR reaches 10 to 15.
Good Samaritan donor — A person who wishes to be a living kidney donor although they do not have a specific person in mind to donate to. These donors are key to the success of donor chain transplants, since their participation enables many transplants to occur. Good Samaritan donors are also known as "non-directed" or "altruistic" donors.
Graft — another word for a transplanted organ. Also called an "allograft".
Hemodialysis — The type of dialysis where a machine cleans the blood of toxins and removes extra fluid. Patients generally require hemodialysis sessions three times a week for several hours each session.
Hepatitis B — A viral infection that affects the liver and can cause chronic liver disease.
Hepatitis C — A viral infection that affects the liver and can cause chronic liver disease. Hepatitis C is the leading indication for liver transplantation in the United States. Within the past several years, Hepatitis C has become a curable disease due to the availability of new treatment regimens that successfully cure more than 95% of patients with the disease.
High blood pressure — A chronic condition (also called hypertension) where the force of blood against your blood vessels is too high. This can lead to kidney, heart, blood vessel, and cerebrovascular disease.
Histocompatibility — A term for the genetic testing and matching that occurs in transplantation.
Human Immunodeficiency Virus (HIV) — The virus that causes AIDS. Patients with HIV can receive a kidney transplant if their HIV is under good control and they are on an appropriate medication regimen for the HIV. Through the HOPE (HIV Organ Policy Equity) Act, patients with HIV can receive organ transplants from deceased donors with HIV infection at participating transplant centers, including our transplant center.
Human Leukocyte Antigen (HLA) — These are the genetic markers present on the surface of our cells that identify us and help the immune system distinguish between our own cells and foreign cells (such as from infection, a kidney transplant, etc.).
Hypertension — Another term for high blood pressure, the chronic condition where the force of blood against your blood vessels is too high. This can lead to kidney, heart, blood vessel, and cerebrovascular disease.
Immune response — The reaction that your immune system has when foreign cells enter the body. This occurs after transplantation, and also when you have an infection, such as the common cold.
Immune system — The body's natural defense against foreign invaders such as infections and transplanted organs. The job of the immune system is to protect us.
Immunosuppression/Immunosuppressant — Another word for anti-rejection medications that transplant recipients must take to suppress the immune system. These medications are needed to protect the transplanted organ from rejection, since the immune system sees the transplant as foreign. Watch the video below to learn more about immune therapy, a technique physicians employ to reduce the chances that a recipient's body will reject its transplanted kidney.
Infection — A condition caused by entry of bacteria, a virus, or a fungus into the body. Transplant patients are more susceptible to infections because of the anti-rejection medications needed to protect the transplanted organ from rejection. However, patients are given medications to prevent the most common infections that occur after transplant.
Informed consent — The process of informing and educating potential transplant candidates and potential living kidney donors about all aspects of the transplant and donation processes, including a detailed description of the risks and benefits.
Islet cell transplant — An experimental (research) procedure for patients with type 1 diabetes mellitus. While less invasive than pancreas transplantation, this procedure is still experimental due to poor long-term function of the islet cells.
No items for this section.
Kidney — The organs in the body that remove certain toxins and extra fluid from the body. Many diseases can affect the function of the kidneys, and patients who developed end-stage kidney disease require dialysis or kidney transplantation to live. It is possible to live with only one kidney (we normally have two), which is why living kidney donation is possible.
Kidney Donor Profile Index (KDPI) score — Each donated kidney has a KDPI score. This is a score from 0-100 that is calculated based on 10 factors about the donor. The score measures how long the kidney is likely to work. A lower KDPI is better. Low KDPI kidneys (defined as a score less than 20) are first matched to transplant candidates with a low EPTS score (see above).
Kidney Paired Donation — A chain of kidney transplants that occurs through a registry of incompatible donor and recipient pairs. By entering a registry, people who have a blood type or crossmatch incompatible donor can exchange donors with other incompatible pairs. Compatible pairs may also participate in order to look for a better age or genetic match for the kidney recipient.
Kidney Exchange — Another term for Kidney Paired Donation (above).
Laparoendoscopic — The method used to remove a kidney from a living donor using minimally invasive surgery through one incision at the umbilicus (belly button). In laparoendoscopic surgery, the surgeon inserts their instruments and camera through the one small incision. The picture transmitted from the camera then guides the surgeon as he or she performs the surgery. The donated kidney is then removed through the same small incision.
Laparoscopic — The method used to remove a kidney from a living donor using minimally invasive surgery. In laparoscopic surgery, several small incisions are made, and the surgeon inserts their instruments and camera through the small incisions. The picture transmitted from the camera then guides the surgeon as he or she performs the surgery.
Liver — A major organ of the body that is responsible for many tasks, including the production of important proteins, cleansing the blood of toxic substances (such as alcohol), breakdown of medications, bile production which aids in digestion, and storage of important substances, like sugar and vitamins.
Living donor — A person who chooses to donate a kidney or part of their liver to a person in need of a transplant.
Match — A term which refers to the genetic matching that is performed between a donor and transplant recipient. Due to the potent anti-rejection medications, genetic matching is not essential to transplantation. A perfect match, however, is associated with better long-term graft survival.
Multiple Listing (also known as "multi-listing") — Being listed for transplant at more than one transplant center. The transplant centers are usually located in different geographic regions.
Never Ending Altruistic Donor (NEAD) Chain — A chain of kidney transplants that occurs through a registry of incompatible donor and recipient pairs. By entering a registry, people who have a blood type or crossmatch incompatible donor can exchange donors with other incompatible pairs. Also known as kidney paired donation or kidney exchange.
Neurogenic bladder — A condition where the bladder does not function normally due to damage to the nerves that normally control the bladder and the flow of urine. This nerve damage can result from various conditions, including diabetes.
Non-Directed donor — A person who wishes to be a living kidney donor although they do not have a specific person in mind to donate to. These donors are key to the success of donor chain transplants since their participation enables many transplants to occur. Non-directed donors are also known as "Good Samaritan" or "altruistic" donors.
NOTA (National Organ Transplant Act) — An act passed by Congress in 1984 that outlawed the sale of human organs for transplantation.
Organ preservation — While organs for transplant are outside of the body (in between being taken out of the donor and placed into the recipient), they need to be preserved to ensure they work as best as possible once transplanted. Some organs are placed in a nourishing fluid and then kept on ice, while others are placed on a machine that pumps nourishing fluid through them while they are waiting to be transplanted.
Organ Procurement Organization (OPO) — Local organizations that are responsible for the retrieval, preservation, and transportation of organs for transplantation. Our local OPO is LiveOnNY.
Organ Procurement and Transplantation Network (OPTN) — OPTN is the unified national transplant network established by the United States Congress to increase the effectiveness and efficiency of national organ sharing and to increase the supply of donated organs available for transplantation.
Pancreas — The organ that produces digestive enzymes needed for the breakdown of food, and insulin, a hormone that allows glucose to enter cells where the glucose is then used as energy for the cells.
Panel reactive antibody (PRA) — A lab test that measures the amount of antibodies that a transplant candidate has in their blood. The higher the number, the more difficult it is to find a compatible donor.
Peritoneal dialysis — A type of dialysis where the peritoneal membrane (which lines the inside of the abdomen) is used to filter waste and extra fluid from the body of a patient with kidney failure. A sugar solution is placed in the abdomen through a catheter and sits there for several hours so that waste and fluid can be removed. The fluid is then drained out through the catheter, and a clean sugar solution is placed in. This process repeats itself multiple times per day.
Pre-emptive kidney transplant — Kidney transplants that occur before a patient requires dialysis. Patients receiving a pre-emptive kidney transplant generally do better than patients who require dialysis prior to their transplant.
Proteinuria — The presence of protein in the urine, which indicates damage to the kidney's filtering system. Watch the video below to learn more about the presence of protein in urine and what it may mean about your health.
Pyelonephritis — A bacterial infection in the kidney which usually results from bacteria traveling from the bladder to the kidney via the ureter. Pyelonephritis is more common in transplant kidneys compared to native kidneys because the length of the transplant ureter is shorter, so there is a shorter distance for bacteria to travel.
No items for this section.
Recipient — This is a term for the person who receives a transplant.
Rejection — Occurs when the immune system recognizes the transplanted organ as foreign and tries to attack it. Most rejections can be treated if caught early. However, each episode of rejection, even if minor, causes damage to the kidney that can affect its long-term function and survival. Rejection is best prevented by taking anti-rejection medications as directed and keeping all follow-up appointments.
Renal artery stenosis — A condition where the blood supply going into the kidney is narrowed. Patients with renal artery stenosis of their transplanted kidney often have a rise in their creatinine and high blood pressure.
Re-transplantation — Transplantation of a patient who has already had a transplant. In most cases, this refers to someone whose prior transplant has failed.
Scientific Registry of Transplant Recipients (SRTR) — This registry is a national (United States) database of statistics related to transplantation. The database includes information about people waiting for transplants and those who have received transplants, and allows the reader to see transplant volumes and survival statistics, which may be helpful to patients who are in the process of choosing a transplant center.
Sensitized/Sensitization — A term used to describe patients who have high levels of antibodies in their blood, which can make transplantation difficult due to risk of rejection. Sensitized patients with a living donor may consider donor exchange in order to find a more suitable donor.
Solitary kidney — A term used to describe a condition where a person has only one functioning kidney due to being born with just one kidney, having a condition where one kidney is non-functional, or when one kidney had to be surgically removed due to trauma or cancer, for example.
Survival rate — Used to describe the percentage of patients alive or percentage of transplants functioning after a designated period of time. You can always find our program’s most recent published survival rates at the Scientific Registry of Transplant Recipients website.
Tissue typing — The process where the blood of the transplant candidate and potential donor are examined for blood type, genetic matching, crossmatch compatibility, and presence of donor-specific antibodies.
Transplant — A procedure where a diseased organ is replaced with an organ from a living or deceased donor.
Transplant Tourism — Traveling to a country outside of the United States (usually to a third world country) in order to obtain a living donor kidney transplant. Transplant tourism is associated with a higher risk of infection and rejection in the recipient of the transplant. This is due to the fact that the management of transplant recipients (in terms of surgical techniques, infection control processes, and medication available to prevent rejection and prevent infection) may be sub-standard.
Transplantation — The field of medicine that deals with transplanting organs from living or deceased donors into transplant candidates who have end-stage organ failure.
United Network for Organ Sharing (UNOS) — UNOS is an organization that facilitates organ matching and placement throughout the United States and also collects and manages data for all transplants that occur.
Ureter — The tube that carries urine from the kidney to the bladder.
Urethra — The tube that carries urine from the bladder out of the body.
Urinary tract infection (UTI) — A bacterial infection that occurs anywhere in the urinary tract (kidney, ureter, bladder).
Urine — The waste product that is produced by the kidneys and stored in the bladder.
Vascular access — A place of entry into a patient's bloodstream that is used during hemodialysis. Types of vascular access include arteriovenous fistula, arteriovenous graft, or temporary catheter.
Waiting list — The list of patients that are waiting for a transplant. Each organ type (for example, kidney, kidney-pancreas, pancreas) has its own list.
Xenotransplant — A term used for cross-species transplantation. Due to the short supply of human organs for transplantation, xenotransplantation has been considered as a potential alternative (for example, transplanting a kidney from a pig into a human).
No items for this section.
No items for this section.