Urinary incontinence (UI), also known as involuntary urination, is any involuntary leakage of urine, whether it is a large amount or just a few drops.
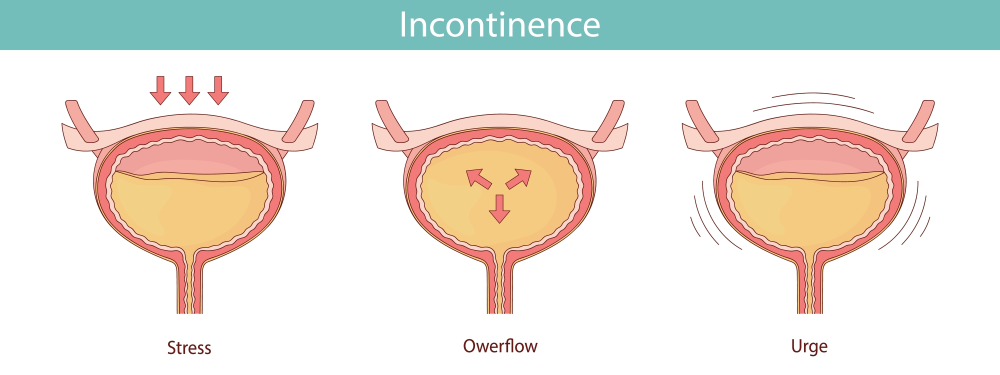
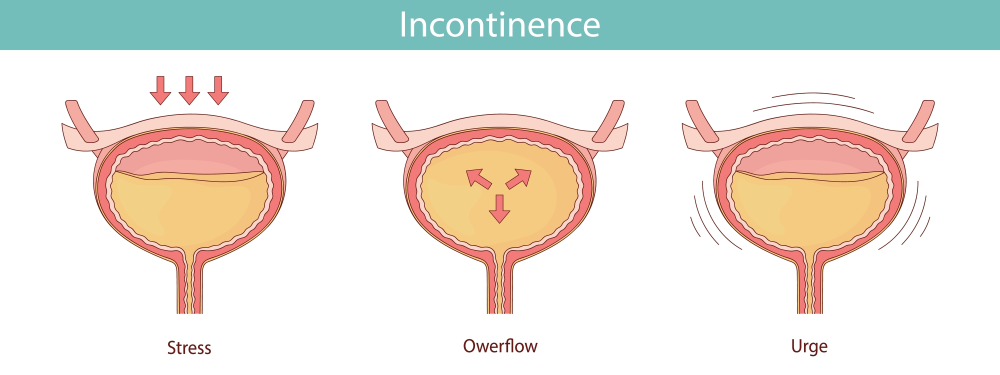
The main types of urinary incontinence include:
1. Stress: leakage with physical activity (for example – with coughing, laughing, sneezing)
2. Urge: leakage preceded by a sudden urge to urinate
3. Mixed: a mix of both stress and urge incontinence
4. Overflow: involves leakage due to a bladder that is too full
Urinary Incontinence Symptoms
Urinary incontinence most commonly leads to the leakage of urine. Symptoms may vary depending on the type of UI.
- Stress: Patients may experience leakage of a small to moderate amount of urine with activity, such as:
o Sneezing, laughing, coughing
o Running
o Heavy lifting
- Urge: Patients may experience a loss of urine immediately preceded by a sudden, strong urge to urinate. They may not be able to make it to the bathroom in time. They may experience incontinence when they hear running water or get close to a bathroom. Certain foods or beverages may make urge urinary incontinence worse as well.
- Mixed: Patients may from symptoms of both stress and urge urinary incontinence. Often, one type seems worse than the other.
Causes and Risk Factors for Urinary Incontinence
Causes of urinary incontinence may include:
- Weak pelvic floor muscles
- Overactive bladder
- Neurogenic) bladder
- Small capacity bladder
- Obesity (which can put excess pressure on the bladder and urethra)
- Chronic cough (which increases pressure on the bladder and pelvic floor muscles)
- Medications
- Aging
- Pregnancy and birth
Prevention Strategies for Urinary Incontinence
Urinary incontinence is common, but it can be managed and even reversed, in some cases. Some ways to help prevent or manage side effect include:
- Avoid or treat constipation
- Quit smoking
- Maintain a healthy weight
- Pelvic floor exercises to strengthen the muscles
- Change bathroom habits
While the likelihood of experiencing urinary incontinence increases with age, it is not considered normal and can interfere with work, socializing, exercise and sexual function. It is recommended to see a doctor if your leakage is bothersome and affecting your quality of life.
Treatment Options for Urinary Incontinence
Both non-surgical and surgical treatment options are available for urinary incontinence, depending on which type the patient is diagnosed with. Patients are given the choice of non-surgical and surgical options depending on the severity of their condition and their personal wishes.
Non-surgical treatment options:
- Kegel exercises: Used to strengthen the muscles of the pelvic floor. These exercises can help control stress urinary incontinence, urge urinary incontinence, overactive bladder and fecal incontinence. In addition, they may be used to help slow the progression of vaginal prolapse. Kegel exercises must be done correctly and regularly to work.
- Pelvic floor therapy: Consists of visits to a physical therapist with specialized training in pelvic floor disorders. These specialized physical therapists utilize a combination of various techniques, listed below, depending on the type of urogynecological condition they are treating.
- Behavioral modification: Consists of education on diet, fluid intake and other lifestyle changes to manage various bothersome symptoms.
- Bladder training: Consists of learning to use the pelvic floor muscles to suppress overactive bladder symptoms, including urinary urgency, frequency, nocturia and urge urinary incontinence.
- Biofeedback: An intravaginal device to train pelvic floor muscles to contract and relax properly.
- Functional electrical stimulation: A device that can be used intravaginally or externally, delivering a gentle electrical current to activate or relax the nerves and muscles in the pelvis.
- Manual therapy: Pressure applied to and released from muscles in spasm to relax them and increase blood flow to the area for healing.
- Joint and tissue mobilization: Gentle manipulation to help calm the muscles and nerves of the pelvis.
- Low-dose vaginal estrogen: Replaces declining estrogen in vaginal and urethral tissues, easing symptoms of vaginal dryness, itching and irritation as well urinary urgency, frequency and incontinence. Low-dose vaginal estrogen comes in a variety of preparations including a cream, suppository or intravaginal ring. This can be used in patients who are peri- or postmenopausal.
- Vaginal pessary: A removable, diaphragm-like device worn within the vagina to support the bladder or other organs that are prolapsing through the vagina. A vaginal pessary may also be used to decrease stress urinary incontinence only. Pessaries come in a variety of types and sizes. Pessary fitting may require two or more office visits to select the proper type and size of pessary.
- Various overactive bladder medications: Helps relax the bladder muscle to allow the patient to store more urine and decrease symptoms of urinary frequency, urinary urgency, and urge urinary incontinence.
Surgical/procedural treatment options:
For stress incontinence:
- Midurethral sling: A small strip of material that is placed beneath the urethra. It provides a firm surface against which the urethra can be compressed during physical activity to prevent stress urinary incontinence. In female patients, this procedure involves a small incision in the vagina. There are a variety of types of midurethral slings. The “gold standard” is to use a small piece of mesh, but the providers can also harvest a portion of the patient’s fascia to be used as the sling called “Rectus Fascial or Fascia Lata Slings.”
- Urethral injections: A transurethral or periurethral injection is a simple outpatient procedure in which a substance is injected next to the urethra to provide support to the urethral sphincter and prevent leakage.
For urgency incontinence:
- Percutaneous tibial nerve stimulation (PTNS): An FDA approved “acupuncture” needle is inserted on the side of the ankle with and a low-dose electrical current gently stimulates the nerve of the tibia. This is repeated weekly for 12 weeks and can lead to decreased overactivity of the bladder.
- Sacral nerve modulation: An FDA-approved treatment for urinary urgency, frequency, urge incontinence and urinary retention. Sacral nerve modulation uses a small device that is implanted under the skin of one of the upper buttocks. It works by gently stimulating the sacral nerves to help the bladder function more normally.
- Botox Injections: An FDA-approved treatment for overactive bladder in which the provide injections Botox into the muscle of the bladder through a camera called a cystoscope.
Would you like an appointment?
To request an appointment, please call our office at (646) 962-7400 or schedule an appointment with one of our providers online below. Our phone staff are available to help you Monday-Friday, from 9AM-5PM (EST).
Meet our expert providers who specialize in treating Urinary Incontinence: