In August 2020, Kim Kittay and her three sons were visiting friends in the Hamptons for the weekend.
On Saturday night, her youngest son, Ezra, wasn’t feeling well. Then, on Sunday morning he seemed fine and spent the day at the beach, but after dinner that evening, he vomited. Kim, her friends and Ezra himself were concerned that it was COVID-19.
At the time, there were no COVID vaccines, and Paxlovid was still a twinkle in Pfizer’s eye. Much less was known about the virus then, but it dominated the headlines along with every conversation people were having. It made sense that COVID would be the first stop en route to figuring out what was going on with Ezra.
Kim’s next guess was that her son had a stomach virus or even food poisoning, possibly traceable to a sketchy breakfast sandwich.
A definitive answer would come a couple of days later. Kim managed to get an appointment with a doctor at Weill Cornell’s West 84th Street location in Manhattan, mainly to get Ezra tested for COVID-19.
Dr. Sherry Huang entered the examination room in full protective gear to administer the test. She also took his vitals, and nothing unusual leaped out at her. He was dry and dehydrated, she recalls—not unusual in the aftermath of several rounds of vomiting. She proceeded to weigh him at the end of the visit, noting that his weight loss was greater than what might have been expected for a 12-year-old boy: He had lost 11 pounds since his last doctor’s visit.
And then came a flash of intuition. Dr. Huang decided to do a urinalysis. And what she found led to a diagnosis that saved the boy’s life.
Ezra’s urine showed high levels of glucose and ketones—substances the body produces when glucose (sugar) is in short supply. It’s called ketoacidosis, an abnormal symptom that points in one direction: type 1 diabetes.
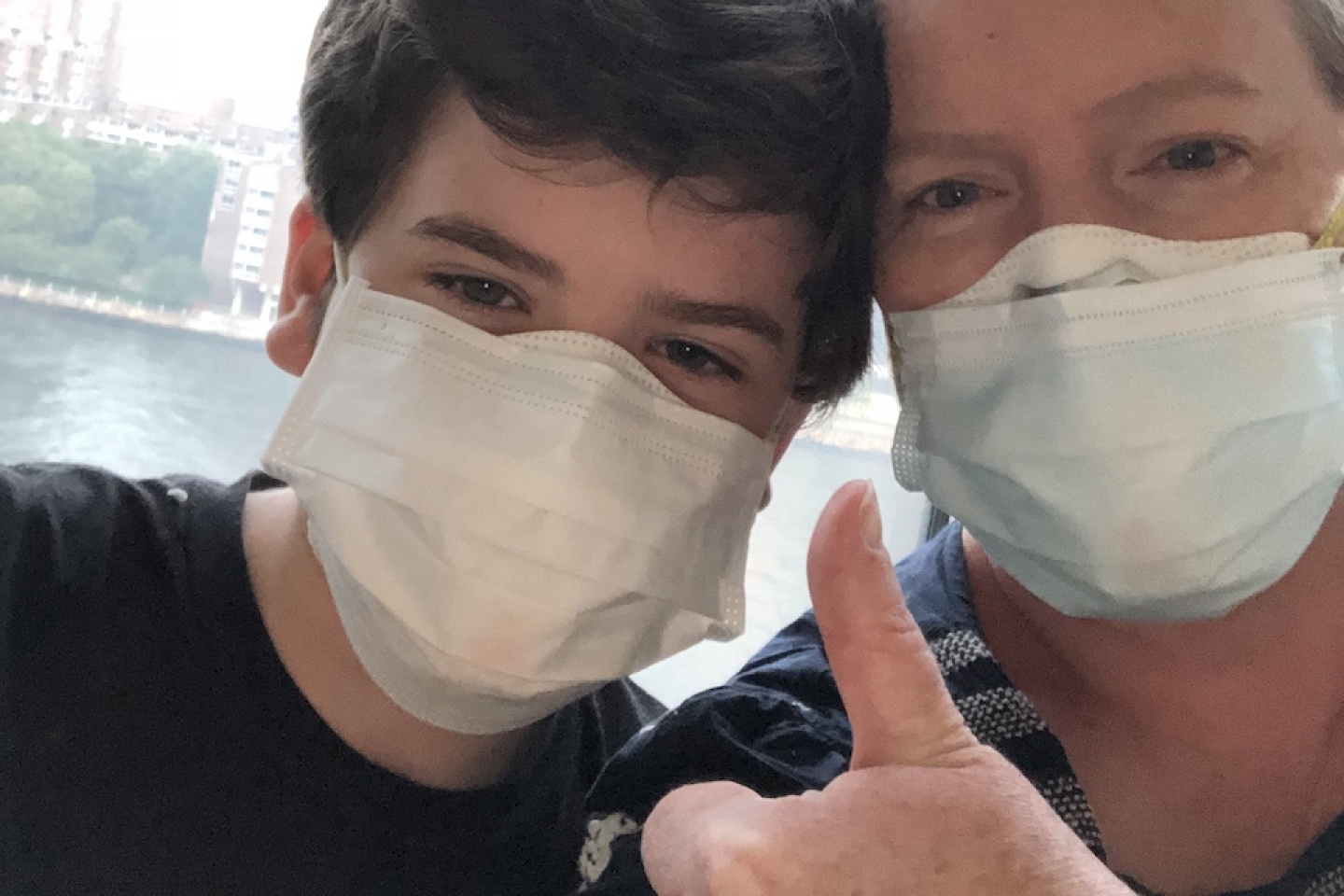
Mother and son had just left the clinic. They were actually on the elevator when they got a phone call asking them to come back immediately. A simple finger prick confirmed it: Ezra’s blood sugar level was off the charts. Dr. Huang urged them to go immediately to the NewYork-Presbyterian Hospital’s emergency room. There, Ezra would receive fluids and glucose, along with support and education regarding his newly diagnosed condition.
“The good news is that it wasn’t COVID,” Kim says. “The bad news is that it was type 1 diabetes, a lifelong condition. But if you have to have one, this is the one to have—especially given the new technologies that monitor and regulate blood sugar and keep everything on an even keel.”
At the hospital, Ezra met with Dr. Zoltan Antal, Chief of Pediatric Endocrinology at Weill Cornell Medicine and an assistant attending pediatrician at NewYork-Presbyterian’s Phyllis and David Komansky Center for Children's Health. Dr. Zoltan went out of his way to tell him, “this doesn’t change who you are.” Ezra replied, “I guess I won’t get to be a judge on Cupcake Wars!”
And speaking of cupcakes, Ezra wondered at first whether his diabetes was his fault, asking: “Did I eat too many sweets?” Every doctor and nurse he encountered responded to his question with an emphatic “no.” Ezra soon learned that diabetes isn’t about punishing children who love candy (his favorite used to be Jolly Rancher).
To this day, Ezra and his mom are grateful to Dr. Antal, who gave them a piece of invaluable advice: Make sure to find a therapist. “He told us that the mental health challenges of having the disease are just as important as the physical challenges,” Kim said. “It’s about treating the whole child.”
Type 1 diabetes (T1D) is believed to be an autoimmune disease, in which the immune system misfires and the body attacks its own organs or tissues. In T1D, that reaction destroys the cells in the pancreas that make insulin.
According to the Centers for Disease Control (CDC), family history and genetics may increase the likelihood that a child, adolescent or young person develops the disease. An environmental trigger, such as a virus, may also play a role.
It can take months or years before T1D symptoms appear. In Ezra’s case, a major symptom—diabetic ketoacidosis (DKA)—sneaked up on him on that fateful weekend. Left unregulated, DKA can be life-threatening, which is why Dr. Huang took Ezra’s condition so seriously.
Dr. Huang has never forgotten Ezra. He was her first patient on her first day on the job at Weill Cornell Medicine. Now, two years later, she uses his case to teach first-year medical school students about an all-important process in clinical care: differential diagnosis.
Doctors use it all the time to home in on what is ailing their patients. For example, what causes vomiting? The first-years crowd around and brainstorm all the diseases and conditions that have vomiting as a symptom, and they go through each possibility in detail, ruling out the most dangerous ones first.
When Dr. Huang saw Ezra back in the summer of 2020, she was able to rule out COVID, food poisoning and a stomach virus. But type 1 diabetes? “That could easily have been missed,” she says. Happily, she caught it in time, and Ezra—now 14—is not just doing well; he’s thriving.
After his 3-day hospital stay, Ezra went home, but the transition was not easy, he recalls. “At the hospital, I got a 3-day crash course in how to manage my diabetes. But a hospital is a controlled environment. There were nurses who could answer my questions, and someone was always on hand to figure out my carbs.”
At home, he struggled with the frequent finger pricks and the tracking of every little thing he ate. Soon, though, technology came to the rescue.
First came Dexcom CGM (continuous glucose monitoring)—a wearable device featuring a water-resistant sensor that is easy to insert. The sensor measures a patient’s glucose levels just beneath the skin’s surface and sends the data wirelessly every 5 minutes to a compatible device such as an Omni Pod. “One device ‘speaks’ to the other,” says Ezra, and that means no more finger pricks, ever!
And as for candy, there are so many zero-carb options available nowadays that he barely misses the sugar-packed variety.
At school, Ezra is active in theater. This May, he performed in a Riverdale Children’s Theater production of Les Miserables. Who needs carbs, he says, when you can sing and dance?