Overview
pH Studies are very important for the correct diagnosis of reflux. Given that antacids are one of the most common over the counter medications and also one of the most commonly prescribed medications it is vital that you get the proper workup prior to long term treatment for reflux either with medications or surgery. You may say that these medications are harmless but more data has come out indicating the many potential hazards of these medications including: cardiovascular, mental function, bone loss, and even early death.
It is unclear what the root cause of these hazards is but some scientists believe it may be due to the alteration of your gut flora since your stomach is not designed to be non-acidic.
As such it is important to have appropriate testing prior to long term therapy. Our group previously published on the over-utilization of antacids and found with appropriate testing nearly one-third of patients on these medications did not meet criteria for these medications.
Therefore, we strongly suggest testing prior to long-term therapy and have two diagnostic tests to help determine if you have reflux.
BRAVO Chip
The BRAVO chip is a device that detects acid reflux. Most patients are recommended to be off different types of medications for up to 2 weeks prior to placement. This chip is placed Endoscopically under light sedations and records your acid reflux for a 2-day period. For the days of the testing you perform all normal activities without restrictions and use the diary and the device to record symptoms and activities. After the study period, we analyze the data and determine if and how significant your reflux is. We can also determine if there are specifics events that can trigger symptoms.
This technique is our preferred method for the diagnosis of reflux as it does not impact your daily activities and is in most cases very comfortable. Less than 1% of patients have difficulty with chest pain from the device.
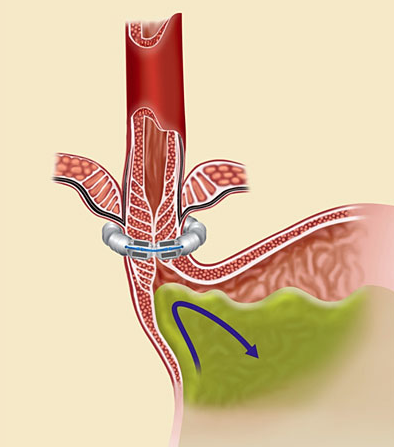
Impedance Probe
The impedance probe is use to detect both acid and weak or non-acid reflux. This is a 24 hour test and involved placing a thin probe in your nose that is attached to a recording device. For the 24-hour of the test you resume all normal activities. The probe can be removed 24 hours after placement. It is more noticeable than the BRAVO probe and is therefore used as second line diagnostic test for reflux. The data can augment the BRAVO data.