Why do I have reflux?
If you have reflux you are not alone.
Gastroesophageal reflux disease (GERD) is a widely prevalent condition, historically affecting approximately 20% of the US adult population. More recently, the prevalence has been estimated to be as high as 40%.
Individuals with GERD present with a variety of symptoms, including:
- Heartburn
- Regurgitation
- Difficulty swallowing
- Hoarseness
- Feeling a lump in the throat
- Excess saliva
- Chest pain
- Bloating
- Early Satiety
- Belching
- Nausea
- Asthma
- Wheezing
- Chronic cough
- Shortness of Breath
- Recurrent Pneumonia
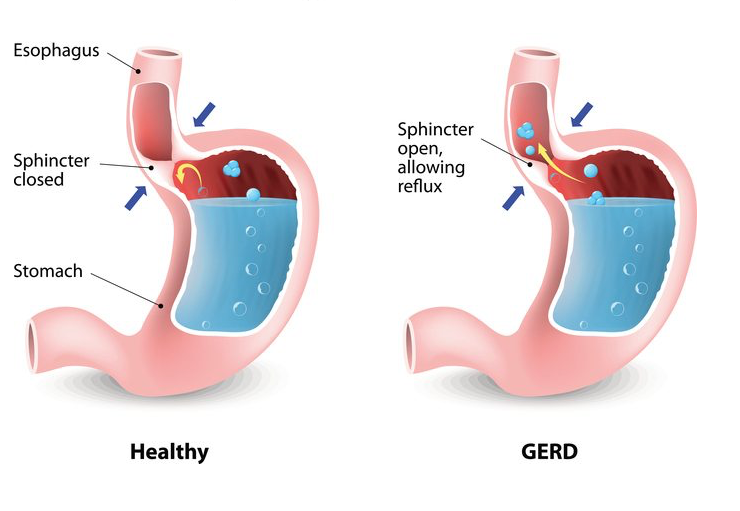
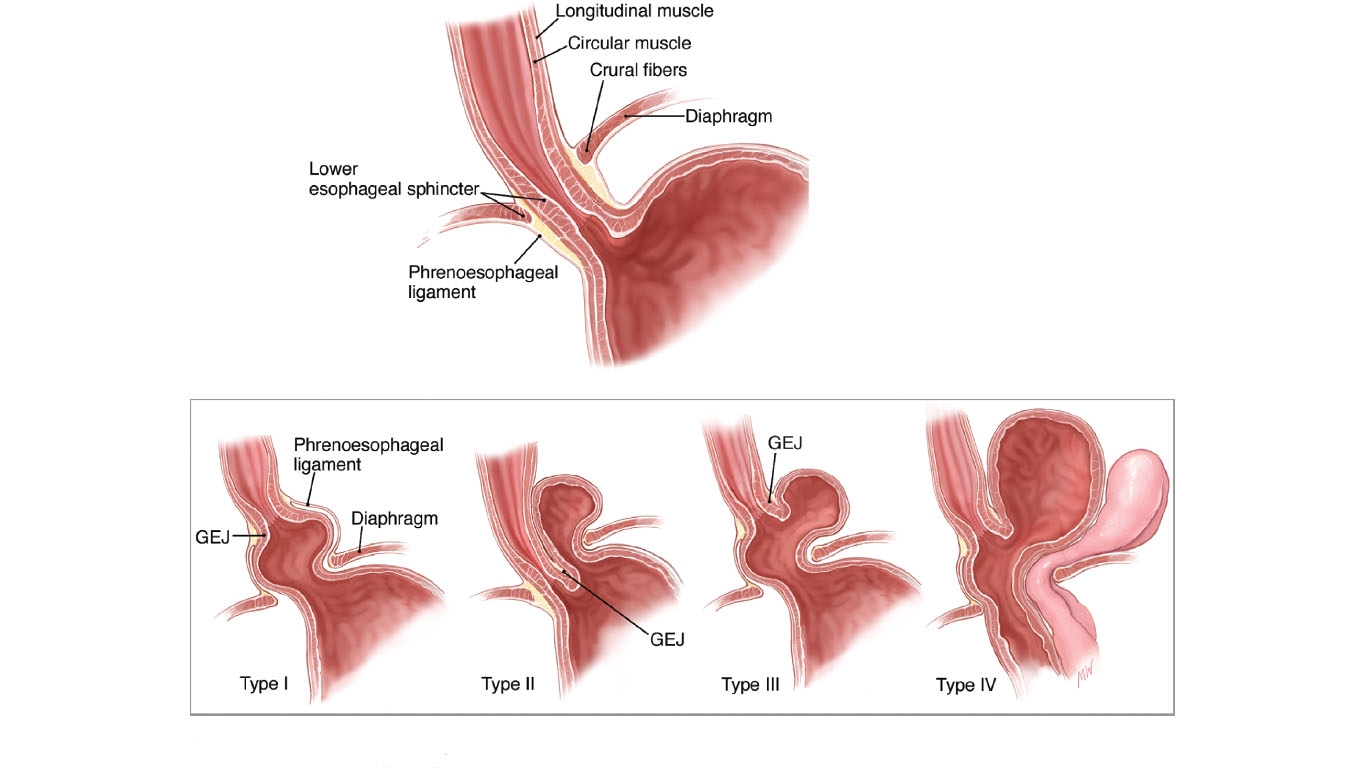
The most common reason to have reflux is that there is a mechanical problem with the valve at is at the bottom of your esophagus. This valve if it is too weak will allow content from your stomach to go into your esophagus and cause symptoms. Sometimes the weakness of this valve is also associated with weakness of the diaphragm so patients also have a part of their stomach that has herniated into their chest. This can make symptoms worse. Because this is a mechanical weakness typically there is no way to strengthen that valve without fixing the problem surgically. However, there are steps to reduce or eliminate symptoms through lifestyle and nutrition modifications.
Causes of Reflux
Most patients with reflux will have classic acid reflux when their valve does not work well. The typical symptoms include heartburn, regurgitation of food and chest pain. Some patient will end up having atypical symptoms including hoarseness, sinusitis, asthma, shortness of breath, throat clearing among others listed above.
Most patients who have these symptoms will end up starting some type of medication including proton pump inhibitors, H2 blockers, or agents that coat the stomach to provide adequate relief. You may even take over the counter medications including Rolaids, Tums, and alike. You still need to have lifestyle and nutrition modifications to help with better outcomes.
Nowadays many of the medications to treat the symptoms for reflux are over the counter and do not need a prescription from your doctor. As such a short trail of these maybe reasonable for some patients suffering with reflux. But some patients may require longer therapy for months or years. In these scenarios, it is important to consult with a doctor with expertise in these disorders to assess your condition and perform if necessary diagnostic testing. Our group has previously shown that up to one-third of patients with reflux symptoms who undergo testing do not have reflux after appropriate testing. Moreover, given that these medications are not benign and can have side effects consideration should be given to how to manage patients to get them the best possible outcome.
Other Causes of Reflux
There are patients that do not have classic reflux that can be difficult to treat. After appropriate testing the major groups for these patients include:
1. Esophageal Hypersensitivity: These patients also have hypersensitivity to small amounts of acid that are normal for most of us. Therefore, the nerve endings trigger at very low levels of acid and therapy should be focused on desensitizing the nerves.
2. Non-Acid Reflux: These patients may have symptoms that correlate poorly with acid and may have other types of reflux including non-acid or bile reflux. Testing for these types of reflux is difficult and most patients in this subgroup are mistreated.
3. Allergy (Eosinophilic Esophagitis): Patients with certain allergies will have esophagitis/inflammation of the esophagus as a major symptom. These patients look very similar to reflux patients but do not have reflux. When biopsies of the esophagus are taken by clinician cells that indicate allergies are present. Allergy testing should be performed.
4. Obesity and Morbid Obesity Procedures and Reflux: Patients with Obesity have reflux as a common symptom. Weight loss can reduce symptoms or alleviate the condition but this is often difficult to do. Therefore, most patient with obesity and reflux will need to undergo bariatric surgery. In the setting of reflux most patients with reflux would be recommended to have a gastric bypass. However, since there are less metabolic abnormalities with sleeve gastrectomy there is a large number of patients that will undergo this procedure.
Moreover, irrespective of prior reflux patients undergoing sleeve gastrectomy will in 40-55% of cases present with new onset reflux.
After appropriate testing this group is ideal for LINX anti-reflux surgery as opposed to conventional approaches including conversion to a R-Y gastric bypass which could impact your metabolism. If further weight-loss is wanted however, the R-Y would offer both reduction in reflux and weight loss while the LINX would only prevent reflux.
Diagnostic Testing
Symptoms alone are insufficient to make the diagnosis of GERD. Most patients will need objective comprehensive diagnostic testing to pinpoint the cause of symptoms. Typically, patient will require at least the following tests to help establish the diagnosis and severity of disease.
Esophagogastroduodenoscopy (EGD): The EGD is the most common test for the initial evaluation of reflux. Most gastroenterologist and clinicians with expertise in this disease can perform this test which is usually done in an Endoscopy Suite and takes a short period of time. Most patients will get some sedation to make them comfortable. Routine biopsies are recommended to determine if there are abnormalities in the esophagus concerning for Esophagitis related to reflux or other causes. Clinicians can also evaluate for Barrett's or other changes that may alter management.
Barium Swallow: This is an X-ray exam where the radiologist will have you swallow liquids, and solids and shoot live images of your swallow to evaluate for anatomic defects in the esophagus and look for signs of reflux, hernia, and masses pressing on the esophagus.
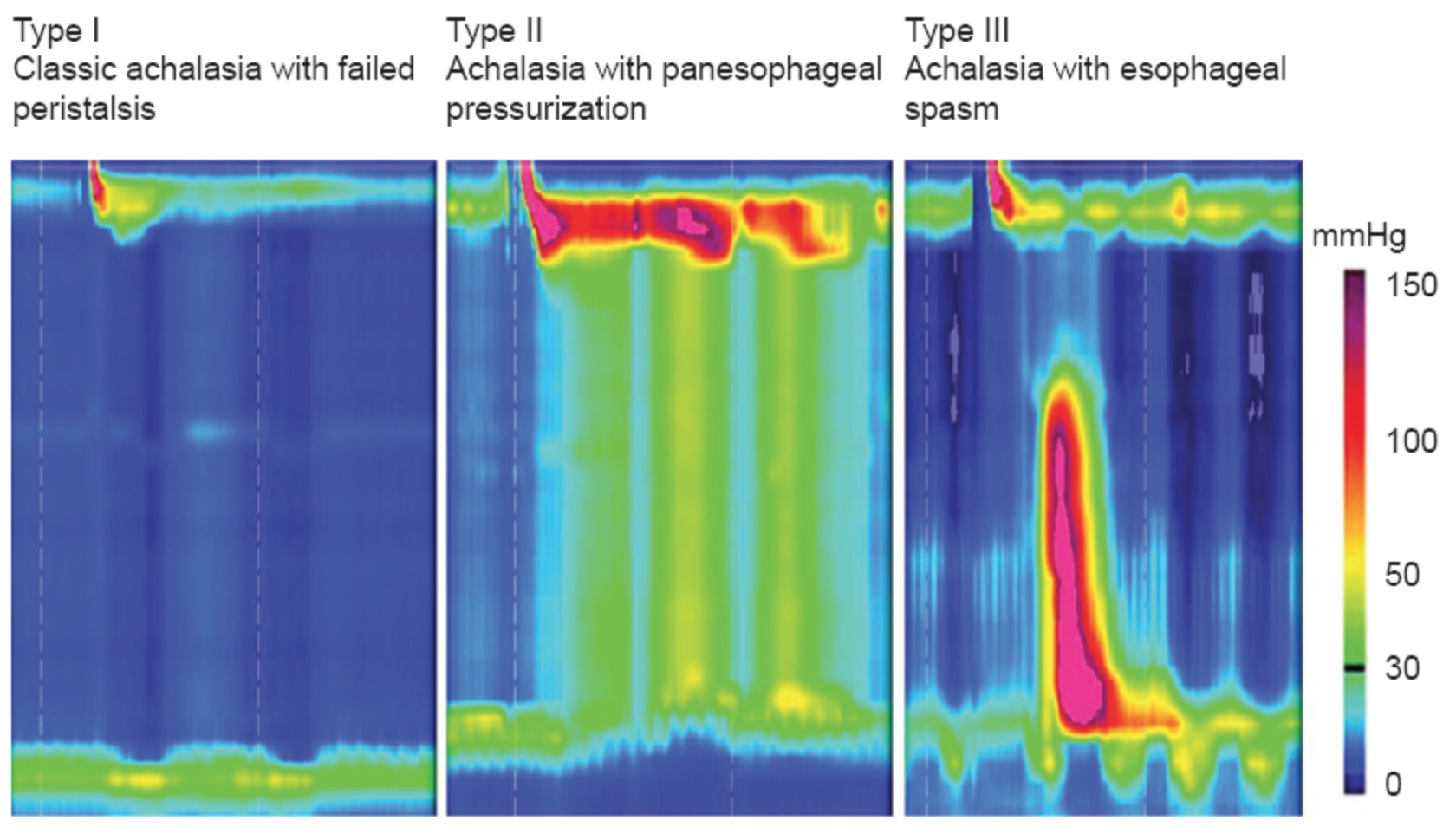
Manometry: This test will determine what the pressures are along your esophagus during swallows. It will detect abnormalities in pressure waves and also function of your valves that may further explain the reason for your symptoms.
pH Study: This test is typically placed by placing a chip in your esophagus that assessing for acid reflux off medications for 48hours. This test is very good for acid reflux but will fail to assess bile or non-acid reflux. In these scenarios impedance testing using a catheter placed in your nose for 24 hours is used. This test is more uncomfortable and is used only in scenarios where acid testing is inconclusive.
Related Treatments