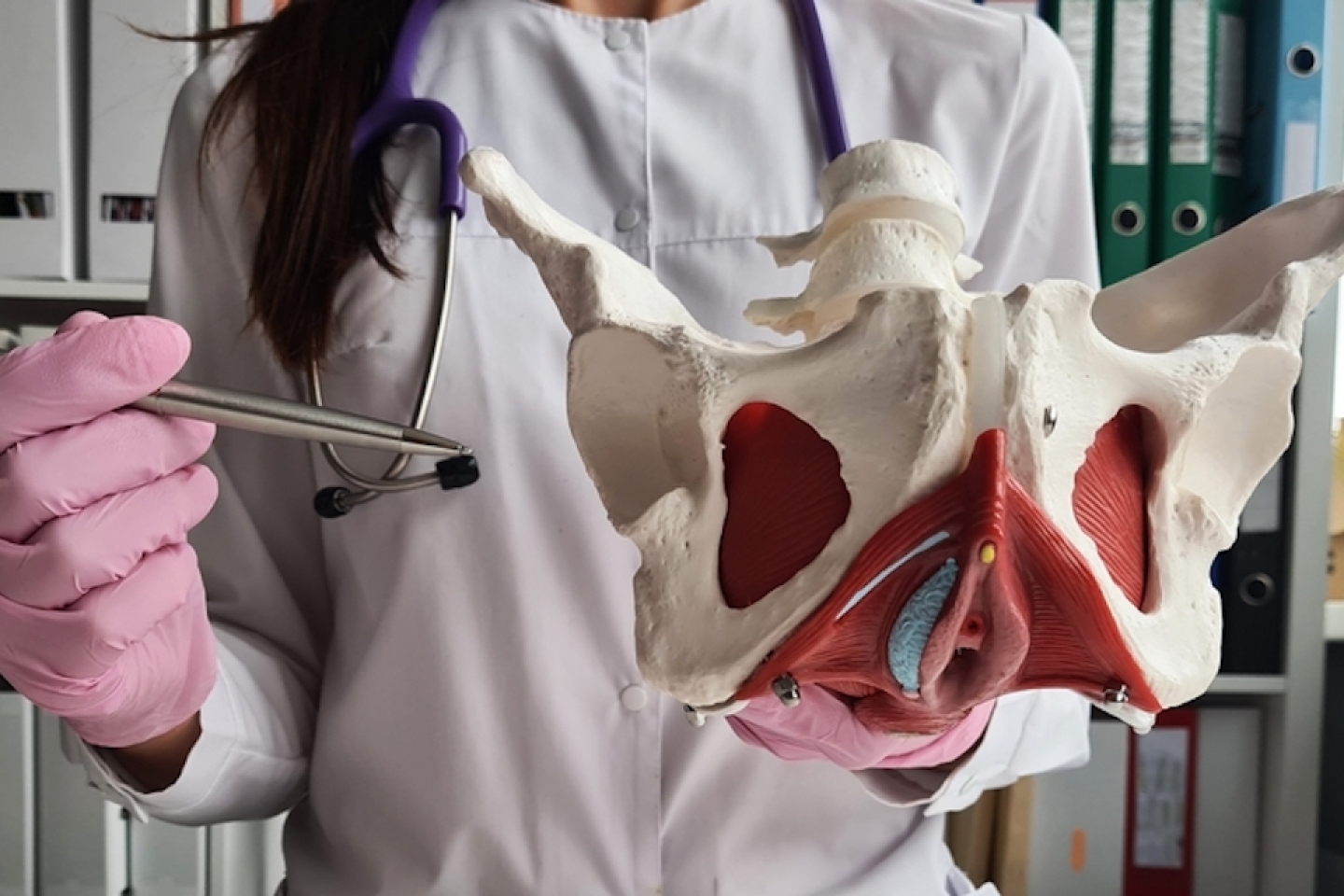
Your pelvic floor consists of muscles and tissues that hold the pelvic organs in place. Childbirth, aging, hormonal changes and more can weaken the pelvic floor over time. When this happens, the pelvic organs may press or fall outside of the vaginal opening resulting in a pelvic floor disorder called pelvic organ prolapse.
One quarter of women experience pelvic organ prolapse in their 40s. Even more women experience it in later years.
“Many women who have prolapse experience it in secret, not realizing how common it is,” says Renee Rolston, M.D., urogynecologist in the Department of Urology at Weill Cornell Medicine. “However, it’s important for women to know they don’t have to live with pelvic organ prolapse. There are treatment options available.”
The bladder is the most common organ involved in pelvic organ prolapse. Other organs involved may include the rectum, uterus and vaginal walls.
When pelvic organ prolapse is present, you may experience the following symptoms:
By not treating the problem, you can experience discomfort during daily activities.
“Pelvic organ prolapse can have a huge impact on quality of life,” Dr. Rolston says. “I’ve had patients stop exercising, not want to go out and cease sexual activity because of prolapse.”
Pelvic organ prolapse is diagnosed during a pelvic or vaginal examination. Based on the stage of your prolapse, your provider will review treatment options which include surgical and non-surgical options.
Your gynecologist or a urogynecologist may provide conservative treatment for pelvic organ prolapse. Regardless of who provides treatment, your options may include:
“Generally, we give patients options, and conservative approaches can help many women,” Dr. Rolston says. “Sometimes, however, we can’t find the correct pessary size. When that happens, we recommend surgery.”
There are two main types of surgery for pelvic organ prolapse reconstructive and obliterative. Both options are minimally invasive and generally are same-day surgery.
Obliterative surgery narrows or closes the vagina altogether, preventing organs from protruding. Sexual intercourse is not possible following an obliterative procedure.
Reconstructive surgery, on the other hand, aims to reposition pelvic organs where they belong. Sexual intercourse is possible following reconstructive procedure.
Types of reconstruction include:
“These surgeries have good results,” Dr. Rolston says. “Also, they’re outpatient procedures, allowing you to return home the same day.”
If surgery is appropriate for you, your care team will help choose the surgery that fits your situation. The type of surgery you undergo depends on factors including:
The goal of pelvic organ prolapse treatment is always the same. Successful treatment reduces symptoms and helps your organs stay where they belong. Providers at Weill Cornell Medicine are eager to help you reach these goals. However, we can only reach these goals when you help us help you. It starts with taking control of your health.
“Many women let embarrassment or fear prevent them from seeking care. This only can allow the problem to get worse. Instead of letting that happen to you, take action,” Dr. Rolston says. “If you see something or feel something abnormal, say something. Talk to your health provider about your symptoms and ask for referral to a urogynecologist. There’s no risk in getting more information and finding out what treatment options fit your circumstances.”
Tired of living with undiagnosed and untreated health issues? Find a doctor at Weill Cornell Medicine to help manage your health.