
If your child needs a specialized medical device to breathe or eat, it’s important to learn how to use it properly. Through Weill Cornell Medicine’s one-of-a-kind Simulation-Based Discharge Program, we will teach you to clean and care for these devices. This way, your child can go home safely and you will have peace of mind.
Weill Cornell Medical Center/NewYork-Presbyterian Komansky Children’s Hospital Patient-Family Advisory Council member Courtney Nataraj knows firsthand the challenges and stress faced by caregivers when transitioning home. As the parent of a child who used medical technology, she was determined to make this journey easier for others. Inspired by her experience, Courtney had the idea that became the Simulation-Based Discharge Program.
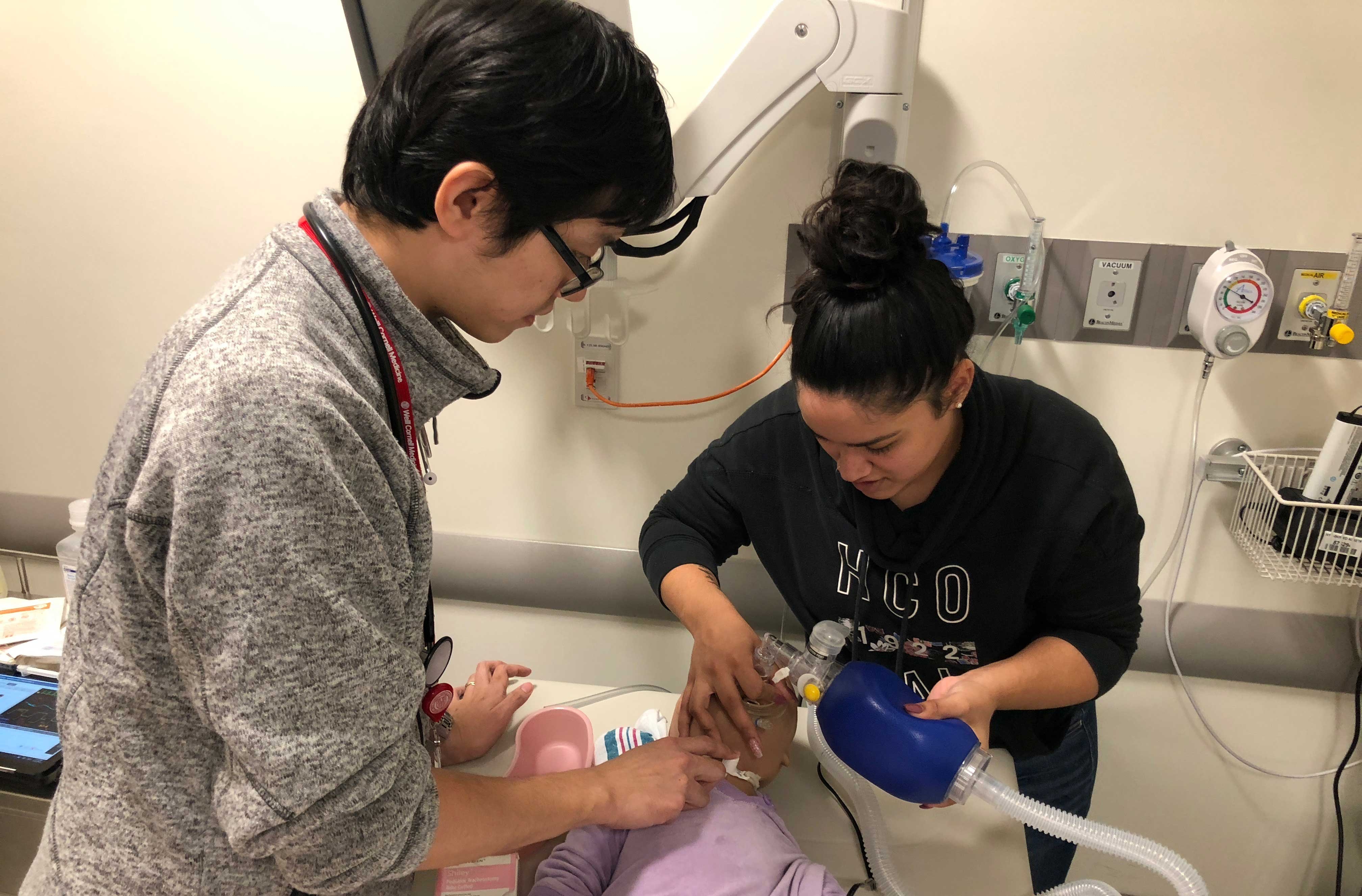
In 2016, her vision took shape when the Weill Cornell Medicine NewYork-Presbyterian Simulation Center, working with Dr. Normaliz Rodriguez, turned her idea into a complete, family-centered training program. Through hands-on learning, the program lets caregivers practice using the device their child will need. This gives them the confidence and skills to safely provide routine care for their children at home.
The Simulation-Based Discharge Program is for all caregivers of children with new tracheostomy or gastrostomy tubes. It gives caregivers the skill and comfort level they need and lessens complication rates for our young patients. The only one of its kind in the area, this program includes two different parts: simulation-based education and peer support.
Before your child is discharged with a new medical device, you will get hands-on experience caring for the device. During this training, you can expect:
Our teaching sessions are made even stronger by the simulated learning resources provided by the Weill Cornell Medicine NewYork-Presbyterian Simulation Center, along with the invaluable expert skills of our dedicated simulation specialists.
Following your child’s discharge, you can view training videos online. They will help keep up your skills and give you even more confidence from the comfort of your home.
Caring for a child with a medical device presents unique challenges. Fortunately, you don’t have to face them alone. Your Weill Cornell Medicine care team is available to answer any questions you may have. You can always reach out to other caregivers as well.
Our Simulation-Based Discharge Program connects you to the hospital’s Family Advisory Council, a parent-to-parent telephone support network. This puts you in touch with others who have been in situations much like yours. You can get advice, encouragement or just talk with others who understand this journey.
This unique support network is yours for six months after your child is discharged.
The Simulation-Based Discharge Program currently serves caregivers of children with tracheostomy or gastrostomy tubes.
For tracheostomy (trach tube), a pediatric surgeon makes a cut in the neck and places a tube inside. This tube opens into the windpipe and helps your child breathe. It also provides a way to clean out mucus and other lung secretions.
A tracheostomy may help if your child experiences the following airway and breathing conditions:
A gastrostomy tube (G-tube) is a soft, plastic tube connected to your child’s stomach through a small surgical cut in the abdomen. This tube allows you to feed your child when chewing or swallowing is difficult or impossible.
Children may need a gastrostomy tube for the following reasons:
Members of the Simulation-Based Discharge Program are specially trained to help you manage pediatric medical devices. Committed to providing families with the best possible care for their child’s tracheostomy and gastrostomy tube needs, our team is here to give you understanding and confidence. This way, you can return home with the knowledge and skills to care for your little one. Members of the team include:
IPFCC’s 25th Anniversary Gala, November 3, 2017, held at the National Press Club in Washington, D.C.
We have had the privilege of partnering with students and experts from local institutions to provide patient-centered, leading-edge teaching.
Two different student teams - from Cornell Tech, Weill Cornell Clinical & Translational Science Center and New York City community organizations - created two separate ways to create affordable, in-house, 3D-printed training models.
To make sure their work would continue and be able to be changed in size, the teams made thorough records of how they did things and shared all digital assets. This way, the staff at the Simulation Center could do the same and take the work even further based on the future, changing needs of the patients.
Students at The City College of New York designed a mobile learning workstation for the NewYork-Presbyterian Hospital Simulation-Based Discharge Program (SBDP). To meet the personalized needs of caregiver teaching sessions, the students designed a mobile workstation for both transport and learning. The colorful outside goes nicely with the pediatric unit’s subway décor theme and adds a playful touch to learning sessions. By becoming more efficient, the Simulation-Based Discharge Program has been able to serve more families.
Our teaching sessions are made even better by the learning resources available through the onsite Weill Cornell Medicine/NewYork-Presbyterian Simulation Center and the expert assistance of our simulation specialists.
Contact the Simulation Center: simulation@med.cornell.edu.
Whether you graduated from Weill Cornell Medicine’s Simulation-Based Discharge Program or are just starting your educational journey, these resources can help as you care for your child with confidence and competency.
![]() Caring for Your Child’s Mic-Key or MiniONE Button Gastrostomy Tube (G-Tube)
Caring for Your Child’s Mic-Key or MiniONE Button Gastrostomy Tube (G-Tube)
![]() Changing Your Child’s Mic-Key Button Gastrostomy Tube (G-Tube)
Changing Your Child’s Mic-Key Button Gastrostomy Tube (G-Tube)
![]() Caring for Your Child’s Gastrostomy Tube (G-Tube or PEG-Tube)
Caring for Your Child’s Gastrostomy Tube (G-Tube or PEG-Tube)
![]() Caring for Your Child’s Standard Gastrostomy Tube (G-Tube)
Caring for Your Child’s Standard Gastrostomy Tube (G-Tube)
![]() Gastrostomy Tube (G-Tube) Frequently Asked Questions
Gastrostomy Tube (G-Tube) Frequently Asked Questions
![]() Pediatric Tracheostomy Care Guide
Pediatric Tracheostomy Care Guide
![]() Guía de Cuidados de la Traqueostomía Pediátrica
Guía de Cuidados de la Traqueostomía Pediátrica
sdp@med.cornell.edu
525 E. 68th St., Box 139
New York, NY 10065