Male Infertility is defined as a couple's inability to achieve pregnancy following one year of appropriately timed and unprotected intercourse.
Infertility is defined as a couple's inability to achieve pregnancy following one year of appropriately timed and unprotected intercourse. By this criterion, it has been estimated that approximately 15-20% of couples attempting to achieve pregnancy are unable to do so. A female factor is the primary etiology in approximately 50% of these couples, and another 20-30% are pure male factor. A combination of male and female factors accounts for the remaining 20-30% of cases. This suggests that in 50% of couples presenting for infertility evaluation, a male factor is contributory. Conservatively estimated, this means that 2.5 million American men would potentially benefit from a fertility evaluation.
The approach to the infertile couple often begins with an evaluation of the female; this is primarily because it is usually the female partner who has initiated a workup by consultation with her gynecologist. As a result, there is often a delay in male evaluation and treatment. The mistaken notion that infertility is associated with "impotence" or decreased masculinity has also contributed to a delay in male evaluation and treatment. It often makes sense, however, to start with the male partner, whose initial evaluation may be performed rapidly and non-invasively.
It is our experience that in 90% of cases, an accurate impression is obtained from an initial visit after a thorough history, physical examination, and light microscopic examination of a semen specimen.
Further testing usually serves to confirm the diagnosis and help direct the course of therapy. Recent research advances in the area of male reproduction have brought about dramatic changes in the ability to not only diagnose, but also treat male infertility. Currently, detection of the underlying problems causing male infertility and directed treatment is possible in most cases.
The specific treatment of male infertility is often more successful, less expensive and possibly less invasive than in vitro fertilization (IVF) or other assisted reproductive treatments. Additionally, about 1% of men who present with the symptom of "infertility" will actually have a serious medical problem causing the infertility that, if left untreated, may jeopardize health or life.
The majority of couples suffering from infertility can be helped to conceive a child. Artificial techniques of reproduction have advanced to the point where a single sperm can be physically injected into an egg (intracytoplasmic sperm injection [ICSI]). ICSI has dramatically changed the treatment available for even the most severe male factor infertility. Because of this technique, 90% of all infertile men, including half of all men with non-obstructive azoospermia, have the potential to conceive their own genetic child.
The human male reproductive system includes hormonal and structural components. These components include the hypothalamic-pituitary-testis axis as well as the epididymis, vas deferens, seminal vesicles, prostate and urethra. Production of spermatozoa requires approximately 3 months from the initial duplication of stem cells that are supposed to develop into sperm, through mitotic divisions and the myriad changes that modify sperm, preparing them for ejaculation and fertilization.
Male fertility is dependent upon the delivery of healthy, viable sperm into the ejaculate. Any disruption in the production, maturation or delivery of sperm can impact a man's fertility. Causes of male infertility can be broken down into defects in sperm production, primary or secondary testicular failure resulting in hormonal abnormalities, obstruction of sperm transport, or a defect in semen delivery.
The condition in which zero sperm is present in a man's semen is called azoospermia which can be divided into two groups called obstructive and non-obstructive azoospermia.
Varicoceles are the most common identifiable condition affecting infertility in men and the most common identifiable cause of secondary infertility. This condition of enlarged veins in the scrotum causes abnormalities in the temperature regulation of the testis. If testicular temperature is elevated by even one degree, sperm production can be adversely effected. Data has shown that the benefit of varicocele repair (varicocelectomy) is related to varicocele size; men with larger varicoceles sustain a greater improvement in semen quality following varicocele surgery than men with small or subclinical varicoceles.
There are various genetic abnormalities that may result in a defect in sperm production or delivery. In fact 10-15% of men with non-obstructive azoospermia may be missing a tiny piece of their Y chromosome (male sex chromosome). This condition is called a microdeletion of the Y chromosome. The Y chromosome carries several genes that are critical for production of sperm. Men who have severely low sperm concentration (including azoospermia – no sperm in the ejaculate) might be missing a small piece of that Y chromosome.
Klinefelter syndrome is the most common chromosomal genetic abnormality that results in a defect in testicular sperm and testosterone production (primary testicular failure). This condition occurs as a result of having an extra copy of the X chromosome. It can affect testicular growth that often results in impaired development of the testes, causing small, hard testicles. This syndrome may result in a myriad of signs and symptoms, which may be present during adolescence or young adulthood or may go unnoticed until men are trying to conceive. Although many men are not detected with this condition until an infertility evaluation, some men have signs and symptoms such as absent or delayed puberty, tall stature, reduced muscle mass, reduced facial or body hair, enlarged breast tissue, low bone mineral density, low energy, decreased libido, or behavioral and psychosocial problems. It is now estimated that roughly 1 in 500-600 males may have Klinefelter's syndrome.
Congenital bilateral absence of the vas deferens (CBAVD) is a structural abnormality that occurs because of an underlying genetic abnormality (CF mutations) causing obstructive azoospermia affecting approximately 1% of all infertile men. Men with CBAVD often test positive for cystic fibrosis gene mutations, although they do not have pulmonary manifestations of this disease. These men are born with the "equivalent" of a vasectomy and diagnosis can almost always be made by a careful physical exam. Sperm production is often normal and men with CBAVD can be helped to conceive by retrieving sperm directly form the epididymis and testicle for use with in- vitro fertilization (IVF) with intra-cytoplasmic sperm injection (ICSI).
Congenital hypogonadotropic hypogonadism occurs when the hypothalamic neurons that are responsible for releasing gonadotropin-releasing hormone (GnRH) fail to migrate into the hypothalamus during embryonic development. This results in the lack of production of FSH and LH, hormones responsible for sperm and testosterone production, respectively. When this is associated with an absent sense of smell or other midline defects, it is called Kallmann's syndrome.
Young syndrome is suspected in men presenting a history of bronchiectasis, chronic bronchitis and sinusitis. This syndrome results in congenital epididymal dysplasia causing obstructive azoospermia.
Primary ciliary dyskinesia (PCD) (immotile cilia syndrome) is an autosomal recessive genetic disorder that causes defects in the action of cilia lining the respiratory tract and the flagella of sperm cells. This results in non-motile sperm. When accompanied by the combination of situs inversus (reversal of the internal organs), it is known as Kartagener syndrome.
Secondary testicular failure is characterized by having low or low-normal gonadotropins (LH and FSH) with a low testosterone level. This condition can be congenital or acquired. Causes of this condition can include kallmann syndrome, prolactinoma, hemochromatosis, empty sella syndrome, or a history of brain radiation therapy. Exogenous testosterone supplementation can also cause this by exerting negative feedback to the hypothalamus and anterior pituitary, resulting in low levels of FSH and LH and impairing spermatogenesis.
Obstruction of the male reproductive tract can result from testicular or scrotal trauma, inguinal or pelvic surgery, prior infection with scarring, ejaculatory duct obstruction or congenital bilateral absence of the vas deferens (CBAVD). Men with obstructive azoospermia will have normal FSH and normal testicular volume.
Retrograde ejaculation is defined by the backward propulsion of semen during orgasm. In these cases, instead of semen being propelled forward out of the tip of the penis, semen is propelled in a retrograde fashion, backwards into the bladder. This is commonly seen in diabetics as well as in men who have had transurethral surgery at or near the bladder neck.
A fertility evaluation is often pursued in couples who have not been able to conceive for a period of 6-12 months of unprotected intercourse. A fertility evaluation may be appropriate sooner than this when the couple is considered to be at higher risk for subfertility or infertility. This includes when the female partner is over age 35, when there has been a history of infertility in a prior relationship or when there are other risk factors which may cause fertility problems (e.g. cryptorchidism, testicular neoplasm, chemotherapy, radiation therapy).
A proper fertility history begins with an assessment of the couple's prior and current fertility status. The age of the partners and the duration of unprotected intercourse is established. It should be ascertained as to whether the infertility is primary or secondary for each partner. If secondary, the nature and outcome of prior pregnancies with the same or any previous partner is necessary. Any previous infertility evaluation or treatment for either partner should be noted as well.
In approximately 5% of couples presenting for infertility evaluation, sexual dysfunction is causative. Is the semen ejaculated into the vagina? Does the couple use lubricants, jellies, oils, or saliva, most of which are known to be spermicidal? Given an approximate 48-hour viability of sperm within the female reproductive tract, timing of intercourse is important. The sexual history should also include an assessment of male libido, which crudely reflects serum testosterone levels.
The man should be questioned regarding the nature and volume of a typical ejaculate. A markedly diminished semen volume and clear, waterlike fluid may suggest absence of the seminal vesicle component associated with either ejaculatory duct obstruction or congenital bilateral absence of the vas deferens (CBAVD). Normal orgasm with low or absent semen volume could also lead one to suspect retrograde ejaculation. Semen that fails to liquefy suggests prostatic dysfunction.
Cryptorchidism means an undescended (hidden) testis. It is present in about 0.8% of newborn males and is an important risk factor for infertility. Hernia repair in infancy or childhood is associated with a 3–17% risk of injury to the inguinal or retroperitoneal vas deferens. Post-pubescent mumps is associated with a 30% risk of unilateral orchitis and a 10% risk of bilateral orchitis, which may result in severe abnormalities in spermatogenesis.
The approximate age of onset of puberty is important. Men will usually remember pubertal landmarks only if they were very early or very late. Precocious puberty suggests an adrenal abnormality such as congenital adrenal hyperplasia. Very delayed or incomplete sexual maturation suggests hypogonadotropic hypogonadism, such as Kallmann's syndrome, or pan-testicular failure, such as Klinefelter syndrome.
Any and all conditions or illnesses for which the patient has been or is currently being treated, including all medications currently or previously taken, are documented. Many prescription drugs interfere with spermatogenesis. Drugs of abuse such as alcohol, marijuana, and cocaine may directly interfere with testosterone and sperm production. A detailed occupational history is directed toward identifying exposure to gonadotoxic agents such as heat, ionizing radiation, heavy metals, and pesticides. A family history directed at fertility problems in parents and siblings may be important. Intrauterine exposure to diethylstilbestrol (DES) is also associated with male genitourinary tract anomalies and dysfunction.
A thorough physical examination can provide insight into the cause of impaired sperm production as well as the overall state of sperm production, and into potential causes of reproductive tract obstruction. The exam is preferably performed in a warm room. The patient's general body habitus and hair distribution are examined.
The breasts are observed and palpated for gynecomastia, which can be associated with an imbalance of testosterone and estrogens, including estrogen secreting testicular neoplasms, adrenal tumors, and liver disease. Nipple discharge or tenderness may be seen with prolactin-secreting pituitary adenomas.
The penis and urethral meatus are also closely examined. The urethra can be milked for discharge. The location of the meatus is noted. Severe hypospadias may result in inadequate delivery of semen into the vagina.
Scrotal examination is first performed with the patient supine. This allows a varicocele, if present, to collapse. Testis size and consistency can then be properly assessed. Normal testicular volume ranges from 15 to 30 cc. The testes should be firm in consistency. A change in testicular consistency is indicative of an abnormality within the testes. In most cases, testes that are normal in size and consistency usually have normal sperm production.
The normal epididymis, which sits behind and to the side of the testis, is normally soft and barely palpable. Hardening, nodularity, or irregularities are suggestive of epididymal pathology, such as obstruction of the reproductive tract beyond the epdidymis.
The vas deferens should be palpated on both sides. The vas is the diameter and consistency of a venetian blind cord, and is usually behind and separate from the internal spermatic cord structures.
With the patient standing, large varicoceles are readily seen through the relaxed scrotal skin in a warm room. Small varicoceles may be appreciated as a distinct impulse and palpable dilation of the internal spermatic veins during the Valsalva maneuver.
If indicated, a digital rectal examination is performed. The size and consistency of the prostate is noted. Masses, cysts, irregularities, tenderness, and whether or not the seminal vesicles are palpable are noted.
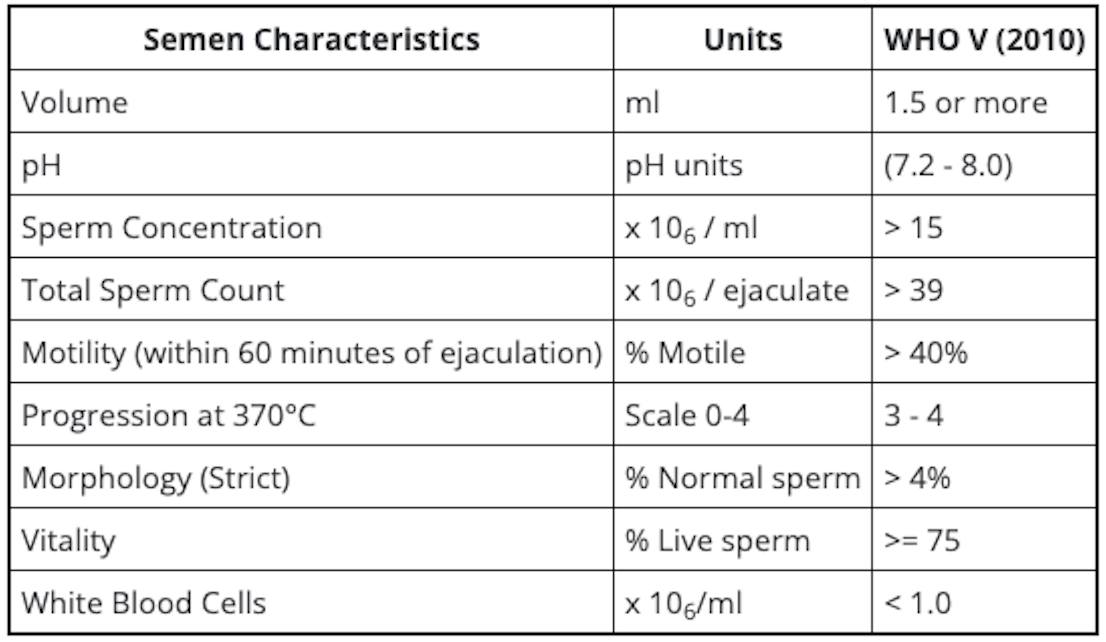
A semen analysis is an imperative part of any fertility evaluation.
Semen specimens are obtained by masturbation into a sterile wide-mouth container after 2-5 days of abstinence and analyzed within 2 hours of collection. Two to three analyses, separated by at least 1-2 weeks, are required for a meaningful evaluation.

Basic endocrine evaluation includes measurement of serum total testosterone (TT) and follicle-stimulating hormone (FSH). Testosterone is necessary for the development and maintenance of secondary sexual characteristics and libido as well as initiation and maintenance of spermatogenesis. Elevated serum FSH suggests abnormalities in spermatogenesis.
It is important for a man of any couple with fertility concerns to be seen and evaluated by a specialist who has experience in treating male infertility.
Treatment of male infertility must be directed towards the underlying etiology. Endocrine abnormalities may be treated with medications to manipulate hormone production. Varicoceles can be corrected using microsurgical techniques. Certain causes of obstructive azoospermia may also be repaired using microsurgical techniques. In other cases of obstructive azoospermia, men may have sperm retrieved directly form the testes or epididymides for use with in vitro fertilization with intra-cytoplasmic sperm injection (IVF/ICSI).
The most exciting, new development in the field of male infertility is the ability to treat men with severe sperm production problems and men with non-obstructive azoospermia. Because pregnancy can be achieved with only one sperm, men with non-obstructive azoospermia can undergo a micro-surgical testicular sperm extraction (micro-TESE) in hopes of finding areas of isolated sperm production. With the advent of ICSI, men found to have even a few sperm may go on to have their own genetically conceived children.
For additional learning on ICSI fertilization processes offered by Weill Cornell Medicine, please visit FertilityIQ.
To request an appointment, please call our office at (646) 962-9600. Our phone staff are available to help you Monday-Friday, from 9AM-5PM (EST).
If you'd like to learn more about our providers that specialize in Male Infertility, please view the "Our Care Team" page.