Benign prostatic hyperplasia (BPH) is the non-cancerous enlargement of the prostate, a walnut-sized reproductive organ. Prostate growth and enlargement are typically seen with aging. In some patients, that growth can block or obstruct the flow of urine. This makes it difficult to empty the bladder, leading to a sense of having to urinate more frequently or with a greater sense of urgency.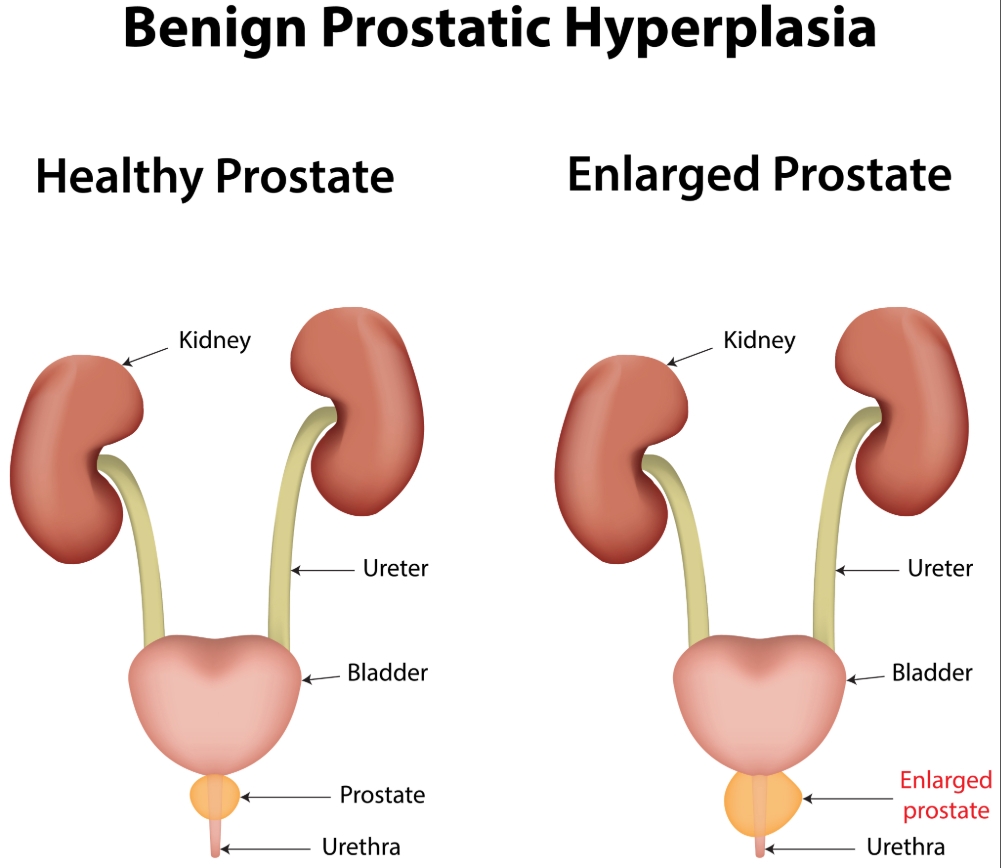
Symptoms of BPH can include:
The exact cause of benign prostatic hyperplasia is unknown.
Risk factors that increase the chances of BPH include:
Importantly, benign prostatic hyperplasia is NOT prostate cancer and does NOT increase the chances of developing prostate cancer in the future.
Evaluation of benign prostatic hyperplasia can include:
o Digital rectal exam (DRE) to check the size and firmness of the prostate
o A urinalysis to evaluate for the presence of infection or any abnormalities
o Postvoid residual to evaluate the amount of urine left in the bladder after urination
o A prostate specific antigen (PSA) test (blood test) to check for prostate cancer
o Blood creatinine to assess how well the kidneys are working
o Urodynamics, or pressure-flow studies, to distinguish whether your urinary symptoms are due to blockage from an enlarged prostate or from a problem with the bladder
o Cystoscopy to evaluate the anatomy of the prostate and to assess for any bladder related conditions.
o Transrectal ultrasound to measure the size of the prostate
Treatment for benign prostatic hyperplasia focuses on reducing its associated symptoms and depends on how bothersome symptoms are. The American Urological Association (AUA) Symptom score is one way to measure how affected you are by your symptoms and how well you are responding to treatment.
o Alpha blockers: Flomax (Tamsulosin), Uroxatral (Alfuzosin), Rapaflo (Silodosin), Cardura (Doxazosin), or Hytrin (Terazosin) relax the muscle around the prostate and bladder neck, increasing urinary flow and decreasing symptoms.
o 5-alpha reductase inhibitors (5ARIs): Proscar (Finasteride) or Avodart (Dutasteride) block the conversion of testosterone to dihydrotestosterone within cells of the prostate, shrinking the prostate size with time that helps reduce the blockage of urine
o Overactive bladder medications: These are a number of medications that inhibit bladder contractions and improve symptom relief
o Cialis: Cialis (Tadalafil) helps to reduce the symptom bother associated with BPH
Surgery is the most effective way to relieve urinary symptoms, but it is typically reserved for situations where medications are not helpful or cannot be prescribed.
To request an appointment or learn more about our program, please call our office at (646) 962-4811. Our phone staff is available Monday through Friday, 9 AM to 5PM (EST).
Meet our expert providers who specialize in Benign Prostatic Hyperplasia: