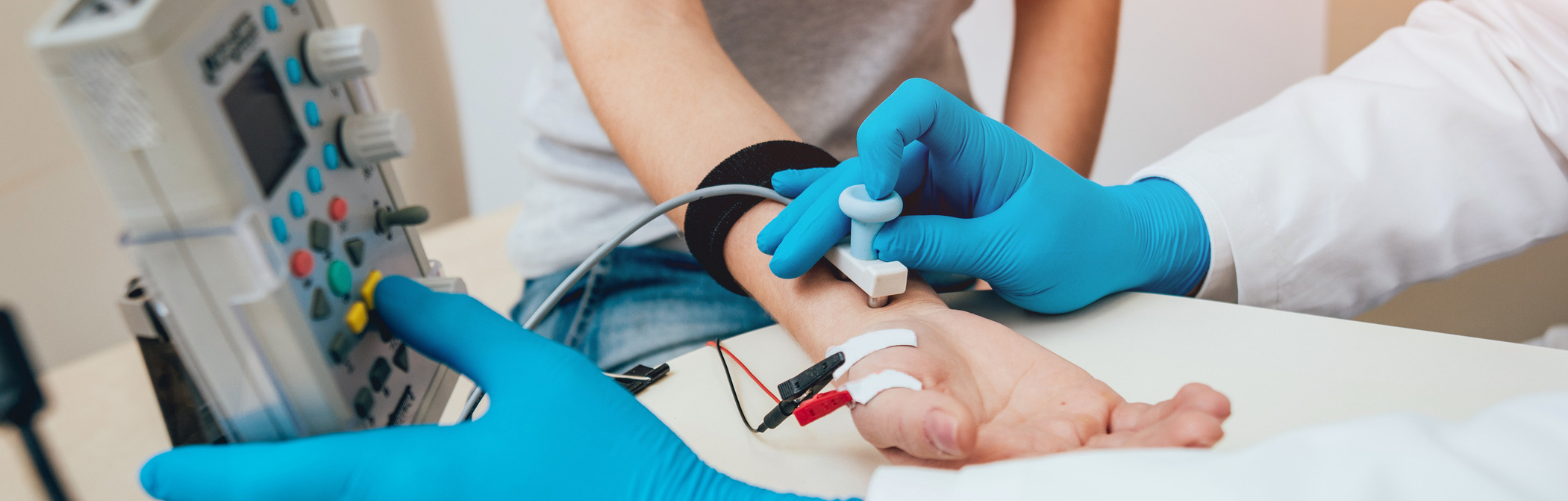
Following a detailed history and neurological examination, patients undergo comprehensive electrodiagnostic testing to determine the presence of a large fiber neuropathy, its distribution, severity, and whether it is primarily demyelinating or axonal. If the EMG and nerve conduction studies are normal, then a punch skin biopsy is done to determine whether the patient has a small fiber neuropathy. Autonomic functions are assessed using QSWEAT, heart rate variability testing, and tilt table testing where indicated.
Patients undergo blood testing for causes of acquired neuropathies, and where indicated, DNA testing for hereditary neuropathies. Tests for acquired neuropathies include those for autoimmune, infectious, metabolic, nutritional, toxic, and paraneoplastic causes. If no cause can be found, and the neuropathy is progressive, then a nerve and muscle biopsy is done, which occasionally reveals the presence of an occult cause such as non-systemic vasculitis, atypical CIDP, amyloidosis, or sarcoid that may be not be detected by the less invasive tests.