Despite overwhelming evidence that the benefits of the COVID-19 vaccine outweigh the risks, and that the chances of dying from the coronavirus far exceed those of having an adverse reaction to the shot, reports of rare, (fewer than one in a million) post-vaccine blood clots may have you reconsidering vaccination.
Before you reconsider, however, you should know that blood clots in the legs (deep vein thrombosis or DVT) or in the lungs (pulmonary embolus or PE), are extremely common and rarely related to the vaccine, according to Maria T. DeSancho, MD, Professor of Clinical Medicine and Clinical Director of Benign Hematology.
Although it is hard to quantify exactly how many people in the United States experience such blood clots, as many as 900,000--1 to 2 per 1,000--could be affected annually, Dr. DeSancho says. “Estimates suggest that 60,000-100,000 Americans die of DVT or PE each year,” she says.
Yet, Dr. DeSancho stresses that your risk of developing a vaccine-related blood clot is no greater than the general population’s overall blood clot risk. “The risk of getting a blood clot either venous or arterial from the COVID-19 vaccines is very minimal compared to the risk in the general population,” she says. Out of 34 million recipients of the AstraZeneca-Oxford vaccine, there were only 169 possible cases of blood clots in the brain, and 53 possible cases of abdominal blood clots; whereas, among the more than 7 million recipients of the Johnson & Johnson/Janssen vaccine, there were just six possible cases of blood clots in the brain, she explains. “The risk of complication is extremely low,” she says.
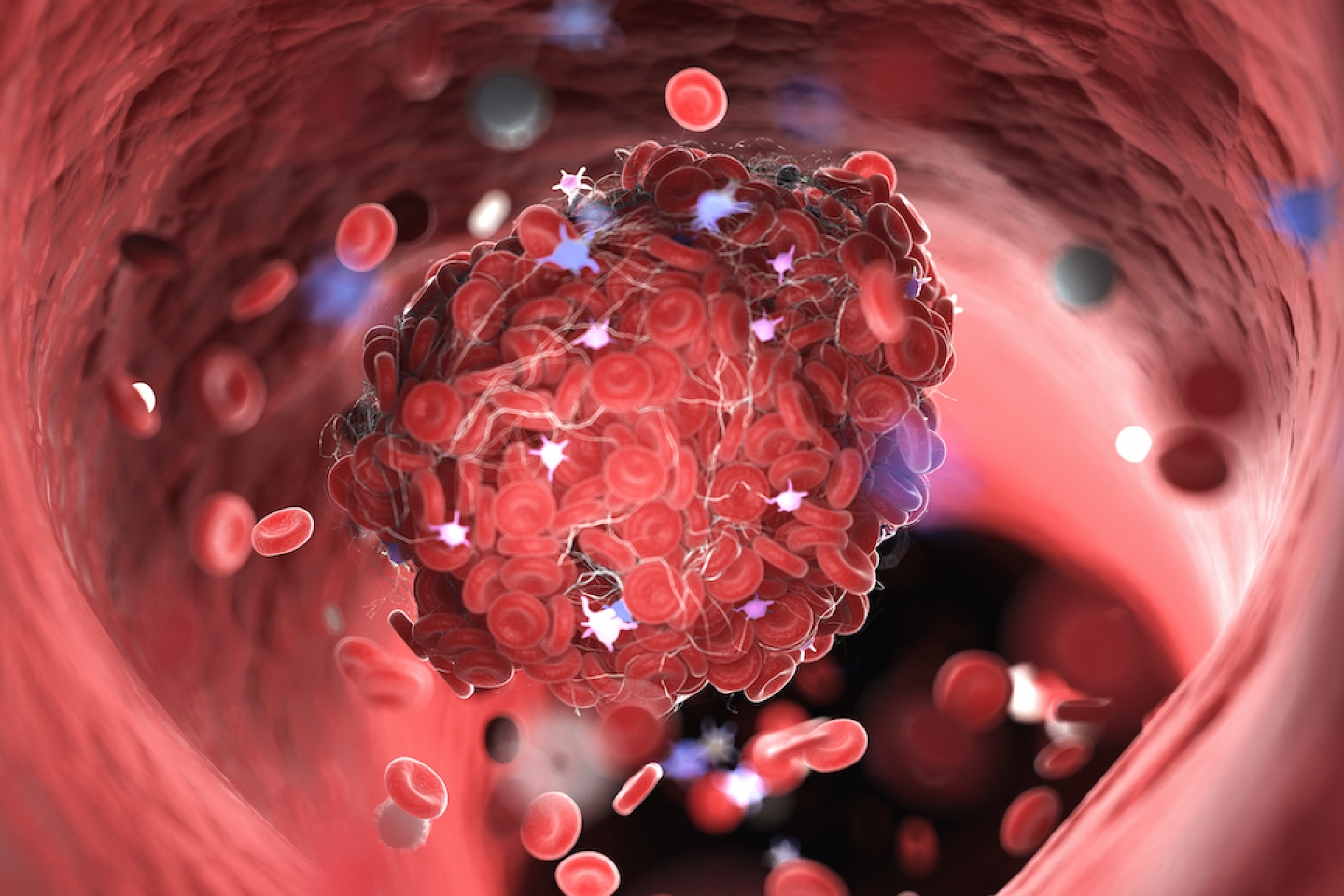
A blood clot is a gel-like clump of blood that forms to stop the bleeding of an injured artery or vein. The platelets in your blood are what help it to clot. (Both the Johnson & Johnson/ Janssen and AstraZeneca-Oxford vaccines are believed to have triggered the production of antibodies that activated the production of platelets, which then caused blood clotting and abnormal bleeding.) Yet, blood clots may also result from illness, genetic disorders, certain medicines, or prolonged immobility. Even COVID can trigger a blood clot.
Blood clots can be stationary (thrombosis) and block circulation. They can also travel (embolism) through your bloodstream to various parts of the body and cause a range of health problems, depending on their size and location. They become more common after age 65, which makes recent incidences of blood clots among some younger vaccine recipients, ages 18 to 48, particularly unusual.
Long hospital stays or periods of bed rest, surgeries (especially orthopedic procedures that involve immobilizing casts), and physical trauma may significantly increase your risk of blood clots. Other risk factors may include:
Symptoms of blood clots depend on where they’re located. For example, blood clots in the legs can cause pain, redness, and swelling, whereas blood clots in the lungs can cause chest pain, shortness of breath, and fainting. In the brain, a blood clot may cause loss of speech or vision, extreme dizziness, or weakness along one side of the body.
Because such symptoms may indicate other health problems, your doctor may conduct various diagnostic procedures, including blood tests, ultrasound, a CT scan, magnetic resonance angiography (MRA) (which looks specifically at blood vessels), or a V/Q scan, (which tests the flow of air and blood in the lungs), to rule out other conditions. If you do have a clot, then your treatment will depend on its location and severity, and may include: