Prostate cancer is the most commonly diagnosed solid organ tumor in men in the United States, with one of seven men developing this disease over their lifetime. In 2017, it is estimated that over 160,000 men will be diagnosed with prostate cancer, and more than 26,000 men will die from it. Prostate cancer is the second leading cause of cancer death in men after lung cancer.
A diagnosis of prostate cancer may lead to anxiety, and the treatment of prostate cancer may affect quality-of-life, with risks of urinary incontinence and erectile dysfunction. However, PSA screening for prostate cancer can decrease the risk of death dramatically. Therefore, a man's age, overall health and life expectancy are critical considerations when considering whether to pursue PSA testing for prostate cancer diagnosis and treatment. The decision to pursue PSA screening and/or subsequent treatment are individualized patient decisions that are best made with the help of a prostate cancer expert.
In recent years, PSA testing alone has been supplanted by a number of secondary tests that can help better determine whether men are at risk of the more aggressive prostate cancers that can cause death. Although detection of prostate cancer requires a biopsy to make a firm diagnosis, blood tests such as the 4kScore test, urine analysis such as PCA3 and imaging using multiparametric prostate MRI can help determine whether a prostate biopsy is even needed. In addition, it is important to remember that many men may have an elevated PSA for other reasons than prostate cancer. In other cases, a diagnosis of prostate cancer may be made, but the cancer may be of such low risk to the patient that the prostate cancer that may be observed rather than aggressively treated, a process referred to as active surveillance.
Early detection is key. The sooner a patient can receive prostate cancer treatment, the better the outcome. Frequent prostate cancer screening can help when it comes to spotting the cancer quickly. If you've recently been diagnosed with the disease, it's important to schedule an appointment with a prostate cancer specialist as soon as possible. Wherever you live in New York— Manhattan, Brooklyn, Queens—Weill Cornell Medicine can accommodate your needs.
Both environmental influences and genetics can predispose men to develop prostate cancer. Since prostate cancer is one of the most genetically-determined cancers, consideration of your family history of prostate cancer (father, brothers affected by disease) is critical to effectively monitor for this disease.
Weill Cornell Medicine is a global leader in prostate cancer research, with notable achievements including identification of the SPOP mutation that is now recognized to create about 10% of all prostate cancers. In addition, our investigators have identified the role of Prostate Specific Membrane Antigen (PSMA) in detection and management of prostate cancers. While several different pathways to development of prostate cancer are evidently present, we know that changes in the DNA of prostate cells can sometimes lead to abnormal development and cancerous growths. Risk factors for such changes include high fat diets, low vitamin D levels and other environmental exposures, in addition to genetics.
A man's age, overall health, prostate cancer histology (Gleason Grade), extent of tumor and life expectancy are critical considerations when considering prostate cancer treatment. In addition to our expertise in robotic prostate cancer surgery, Weill Cornell Medicine offers expert care for patients in New York under active surveillance (also known as watchful waiting), minimally invasive therapies including High Intensity Focused Ultrasound (HIFU) and cryotherapy, as well as state-of-the-art radiation therapies & chemotherapy. The decision to pursue and select treatment(s) is an individualized one that our experts in this condition are available to help guide you through. We have a multi-disciplinary team for patient care that involves world-leading experts in surgery, minimally invasive therapies, radiation and other approaches including our experts in medical (urologic) oncology, urology, radiology, pathology and radiation therapy.
Learn more about the Multidisciplinary Prostate Cancer Clinic.
Prostate Cancer: Know The Facts Infographic
RP Surgical Approach compilation 20211227
Older age is a risk factor for prostate cancer. Autopsy studies have shown that 30% of men in the 5th decade of life have evidence of prostate cancer versus 50% of men in the 8th decade of life. In the United States, 60% of men with prostate cancer are diagnosed after the age of 65 years.
Prostate cancer is also diagnosed more commonly in African-American men compared to white men. In addition, it is less commonly diagnosed in Asian men and Hispanic/Latin-American men compared to white men. Although reasons for this variation in prostate cancer incidence by race remain unclear, it is thought that differences in animal protein and fat intake may contribute.
Obesity is also associated with a higher incidence of prostate cancer. Family history of prostate cancer in a primary relative (biologic father and/or brother) has also been implicated in contributing to a greater risk of prostate cancer.
In the below video, Dr. Christopher Barbieri highlights the importance of genetic testing to help assess one's risk of prostate cancer and how agressive the cancer may be.
In the below video, Dr. Christopher Barbieri discusses how genomics and DNA repair defects play a role in an individual's risk of developing prostate cancer, and furthermore, how the indentification of specific molecular sub-types of prostate cancer can impact individual treatment paths.
While direct causes for the incidence of prostate cancer remain unclear, research suggests that an individual's age, race and body weight all have impacts on the likelihood of diagnosis. You can learn more about your specific risks from a urologist at Weill Cornell Medicine.
For men with an abnormal PSA, there are now additional tests that may be considered before prostate needle biopsy. These include prostate Magnetic Resonance Imaging (MRI) and other genomic tests such as the 4k test and the Prostate Health Index (PHI).
At Weill Cornell Medicine, we utilize a 3D imaging device in order to fuse an MRI scan of the prostate with an ultrasound image in real time. This allows the urologist to accurately pinpoint areas of interest within the prostate and target biopsy needles to take samples from these specific areas. Additionally, this allows us to sample the exact locations again in the future if the patient returns for a follow-up biopsy, yielding precise tracking of any cancer progression.
If prostate cancer is detected, it is stratified into risk categories of low, intermediate and high risk.
Additional work up with imaging (bone scan, CAT scan or MRI) and treatment options are based on a man's prostate cancer risk stratification.
Learn more here about having an MRI or CT scan performed at Weill Cornell Medicine.
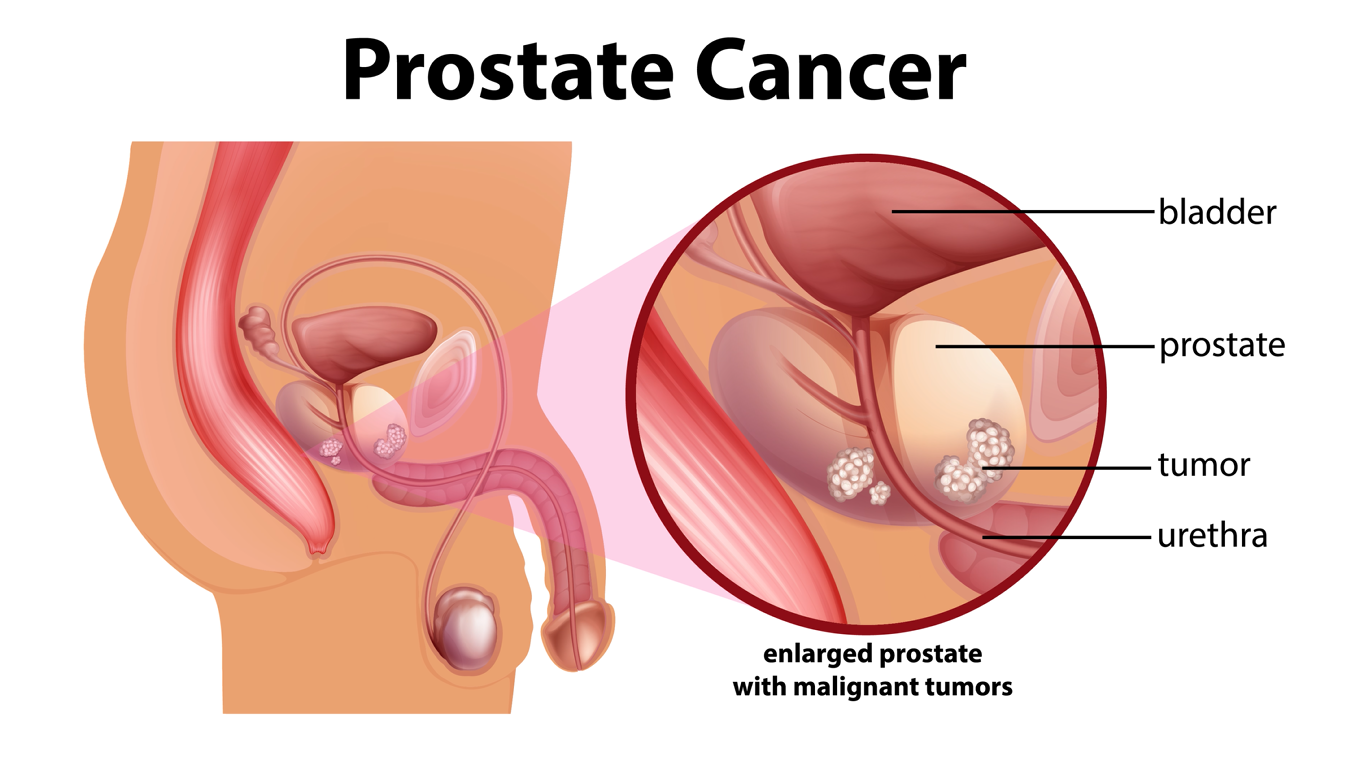
Locally advanced prostate cancers may obstruct urinary flow and/or cause severe irritation in the bladder region when the cancer extends from the prostate into the base of the bladder. Treatment of this locally advanced cancer can be very difficult. Obstruction to urinary flow may be opened by transurethral resection of the prostate, but there is a delicate balance between opening the urethra adequately to void, and opening the urine passage too much, resulting in incontinence.
An individual's treatment path for prostate cancer is determined after assessing the risk level of your disease. Treatment paths are also greatly influenced by age and lifestyle of an individual with prostate cancer. For example, a 40 year old man diagnosed with early stage & low-risk prostate cancer may still decide to opt for a robotic prostatectomy to eliminate lifelong surveillance / watchful waiting. Then again, another 40 year old man may choose to forgo active treatment and regularly monitor to check for progression of the disease. For men with high risk disease, multi-modal therapy is usually needed, as surgery or radiation therapy alone may not be curative.
New and emerging technologies utilized at Weill Cornell Medicine allow us to more accurately follow patients on active surveillance and provide effective treatments through minimally-invasive & non-surgical therapies. The multidisciplinary emphasis within our prostate cancer program gives us an edge for accurate diagnosis and enables us to provide all treatment options, including surveillance, image-guided therapy, radiation and surgery.
When is a radical prostatectomy recommended for men with prostate cancer?
If you would like an appointment, please call us at (646) 962-9600. Dr. Jim C. Hu goes over some common questions many men have about prostate cancer surgery, a.k.a. radical prostatectomy.
Men with low risk prostate cancer may choose from the full spectrum of radiation therapy options, including brachytherapy (radioactive seeds), intensity modulated radiation therapy (IMRT), proton beam therapy, or combination therapy
Prostate cancer grows in response to testosterone. Testosterone is produced in the testicles and the adrenal gland. Testosterone production can be stopped in two ways.
For men with hormone-resistant prostate cancer growth, several options, including investigational treatments, are available through clinical trials. Most men treated for hormone-resistant prostate cancer have symptomatic disease.
Cryo-Ablation, or Cryotherapy, is a minimally invasive treatment that involves targeting freezing of cancerous tissue within the prostate. Using needles called cryoprobes, prostate tissues are repeatedly frozen and thawed in order to kill the cancerous tissue. Cryo-Ablation can be performed either as a whole-gland or partial-gland procedure. Whole gland cryoablation is used when the cancer is evenly distributed and spread across the entire prostate. An advanced procedure, called focal cryoablation allows the surgeon to utilize location data from biopsies to guide & target the needles to kill only the specific parts of the prostate that are cancerous. This allows the prostate to remain intact while the cancerous sections are destroyed.
High Intensity Focused Ultrasound (HIFU) is a minimally-invasive and non-surgical therapy that utilizes focused ultrasound waves to heat and destroy prostate tissue. During a HIFU treatment, an ultrasound probe is placed inside a man's rectum and aimed towards the prostate. Just as intensified light can cause powerful heating, focused ultrasound waves create heat that is used to kill specific tissues within the prostate.
HIFU may be performed either as a whole gland or partial gland procedure. In a partial gland HIFU, the ultrasound waves are focused on the specific portions of the prostate that were identified of concern. In a whole gland HIFU, the entire prostate is targeted.
Learn more here about the High Intensity Focused Ultrasound (HIFU) procedure provided at Weill Cornell Medicine. Learn more here
For information on the clinical trials currently open at Weill Cornell Medicine for prostate cancer, please visit the Joint Clinical Trials Office website.
To request an appointment, please call our office at (646) 962-9600. Our phone staff are available to help you Monday-Friday, from 9AM-5PM (EST).
If you'd like to learn more about our providers that specialize in Prostate Cancer, please visit the "Our Care Team" page.