Kidney stones (nephrolithiasis) are small, hard mineral deposits that form inside the collecting system of the kidneys.
Kidney stones affect up to 5% of the population, with a lifetime risk of passing a kidney stone at about 8-10%. While more common in warmer southern states, they are a frequent reason for patients to seek urologic care in the northeast. Stones form twice as often in men as women. The peak age in men is 30 years; women have a bimodal age distribution, with peaks at 35 and 55 years. Once a kidney stone forms, the probability that a second stone will form within five to seven years is approximately 50%.
Kidney stones are small, hard mineral deposits that form inside the collecting system of the kidneys. These stones form when the urine becomes concentrated, allowing the minerals to crystallize and adhere to one another. The most common minerals are calcium, oxalate, phosphate and acid salts. This may occur due to several reasons including dehydration, dietary factors, chronic urinary infection, and less commonly, an underlying metabolic disorder. They form within the kidney but may affect any part of the urinary tract including the kidneys, ureters and/or bladder.
When you are diagnosed with a kidney stone, it is important to have a urologic evaluation in order to discuss your symptoms and management of the stone. Our specialists are available to provide an evaluation, as well as any needed follow-up treatment.
Once the stone has passed or been removed, it is important to determine your risk factors to minimize the chances of more episodes.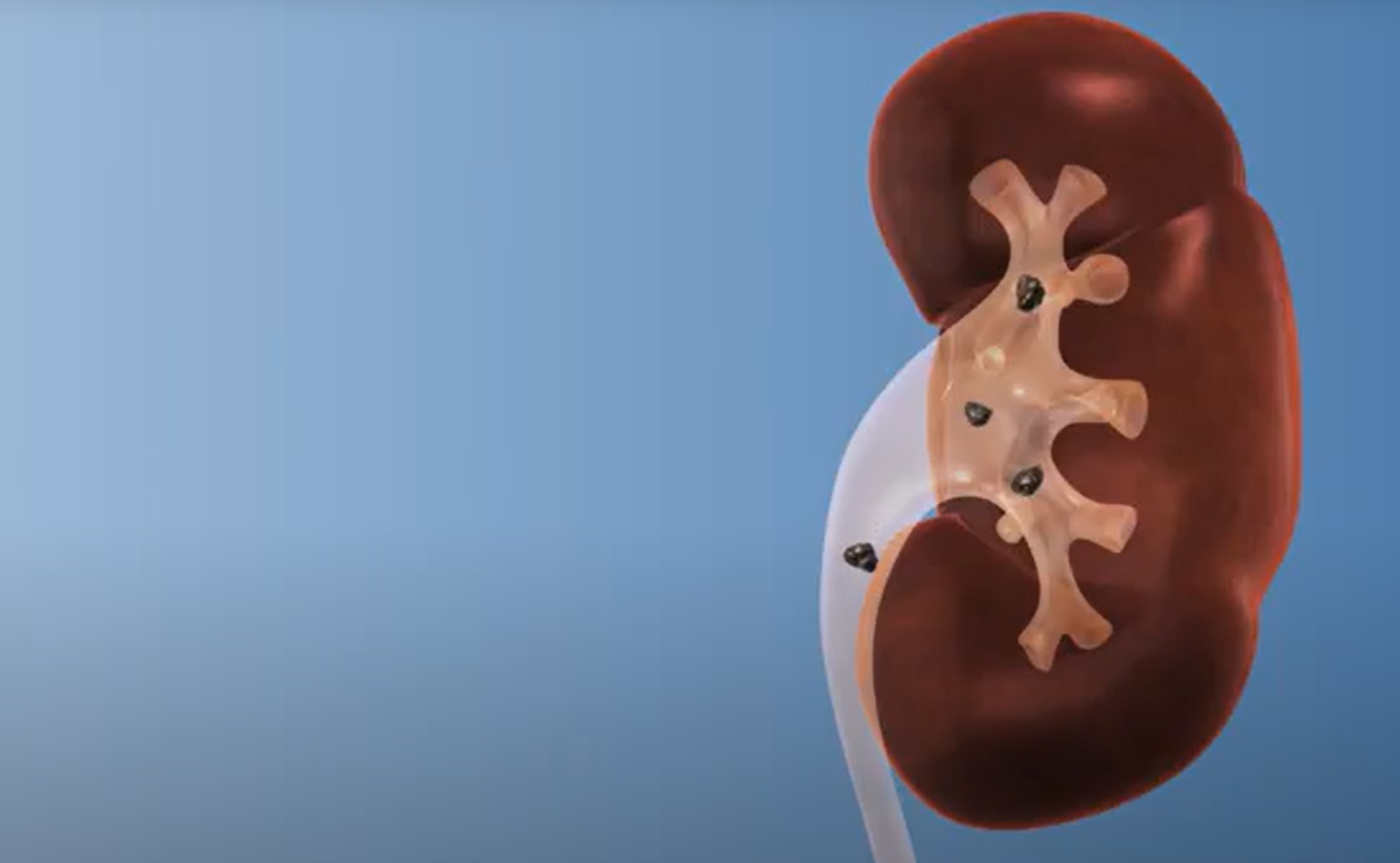
Factors that increase your risk of developing kidney stones include:
Dehydration: This is the most common cause and the easiest to remedy. Kidney stones form when your urine contains more crystal-forming substances than the fluid in your urine can dilute. Therefore, not drinking enough water each day can increase your risk of kidney stones.
Diet: Studies have shown that eating a diet that's high in sodium can increase your risk of certain types of kidney stones. Too much sodium in your diet increases the amount of calcium your kidneys must filter and significantly increases your risk of kidney stones. In addition, diets that are high in protein and sugar can increase your kidney stone risk. At the same time, your urine may lack citrate, which is known to prevent crystals from being able to adhere to one another, creating an ideal environment for kidney stones to form. For most patients, a low-protein, low-sodium, and moderate-calcium diet is recommended. Specific dietary recommendations will be based upon your stone composition and evaluation of your metabolism.
Family or personal history: If someone in your family has had kidney stones, you're more likely to develop stones than someone without a family history.
Obesity: High body mass index (BMI), large waist size, and weight gain have all been associated with an increased risk of both a single episode and recurrent episodes of kidney stones.
Digestive diseases and surgery: Certain disorders of the digestive system can affect calcium, electrolyte, and water absorption, which may increase your risk of forming kidney stones. Common disorders include gastric bypass surgery and inflammatory bowel diseases, such as Crohn's disease and ulcerative colitis.
Metabolic disorders: Metabolic conditions that may increase your risk of kidney stones include renal tubular acidosis, cystinuria, and hyperparathyroidism.
Urinary tract infections: Patients who suffer from chromic urinary tract infections may form larger stones up in the kidney. These are commonly called struvite or infection stones.
Other Risk Factors:
Anatomical abnormalities
Obstruction of the kidney or ureter
Calyceal diverticulum
Horseshoe kidney
Ureterocele
Vesicoureteral reflux
Ureteral stricture
Medullary sponge kidney
Types of Kidney Stones:
Knowing the type of kidney stone helps determine the cause and may give clues on how to reduce your risk of getting more kidney stones. This is why it is important to attempt to collect the stone for analysis.
Calcium stones: Most kidney stones are calcium stones, usually in the form of calcium oxalate. Oxalate is a naturally occurring substance found in food. Some fruits and vegetables, as well as nuts and chocolate, have high oxalate levels. Dietary factors, high doses of vitamin D, intestinal bypass surgery, and several metabolic disorders can increase the concentration of calcium or oxalate in urine. Calcium stones may also occur in the form of calcium phosphate.
Struvite stones: Struvite stones form in response to urinary tract infection. These stones can grow quickly and become large. If not treated, they can alter function of the kidneys over time.
Uric acid stones - Uric acid stones can form in people who are dehydrated, eat a diet high in protein, or those who have gout.
Kidney stones typically do not cause symptoms while they form within the kidney. If the stone passes into the ureter – the narrow tube that connects the kidneys to the bladder – it may cause pain if/when it gets lodged in the tube. Pain caused by a kidney stone may change to a different location or increase in intensity as the stone moves through your ureter. The pain from the stone is not from it moving down the ureter, but rather from the blockage it is causing, reducing the kidney's ability to drain properly. Therefore, the pain may lessen or disappear when the stone changes location within the ureter to a position where it is not blocking the flow of urine from the kidney towards the bladder.
Common Symptoms and Signs That You May Experience:
Severe pain in the side and back that comes in waves and fluctuates in intensity
Pain that may radiate to the lower abdomen and groin
Nausea and vomiting
Pain with urination
Pink, red, or brown urine
Persistent urge to urinate
Fever and chills if an infection is present
Cloudy or foul-smelling urine if infection is present
In many instances, pain from passing a stone will occur suddenly. Patients should contact their physician right away when this occurs.
Immediate medical attention is required when pain is:
So severe that a comfortable position can not be found
Increasing despite analgesics
Accompanied by nausea and vomiting
Accompanied by fever and chills
Evaluation:
In many instances, your doctor may instruct you to go to the emergency room for prompt evaluation. In addition to detailed history, including family history of stone disease and past history of stone passage, the basic investigation into a patient who is passing a stone are:
Vital signs, including temperature, blood pressure, and heart rate
Urinalysis, including urine pH and urine culture
Serum blood counts to assess for possible infection
Serum electrolytes (calcium, phosphate, bicarbonate, uric acid)
Blood urea nitrogen, serum creatinine (renal function)
Radiologic investigation (options):
Unenhanced helical computed tomography (no dye) is the best imaging method to confirm the diagnosis of a urinary stone in a patient with acute flank pain. The accuracy is greater than 95%. It also gives specific information about the density of the stone and the location, which helps guide the physician with treatment options.
Ultrasound (sonogram) has the advantage of having no associated radiation but it is less accurate in the acute setting. It can be used to monitor the kidney and the stone during attempted passage.
Plain abdominal x-ray (KUB – Kidney/Ureter/Bladder) is important to assess the radio-opacity of the stone, to monitor stone progression, and to determine potential therapy.
Metabolic evaluation:
In a patient with recurrent stones, in addition to the baseline investigations, a 24-hour urine assessment should be done for urine volume and calcium, oxalate, uric acid, citrate, urine sodium, and creatinine excretion. Urine creatinine is measured to determine the accuracy of urine collection. This is not done during the acute management of a stone, but rather afterwards to try to optimize fluid intake and dietary adjustments to prevent recurrent stones from forming.
Treatment of your kidney stone depends on several factors that are specific to your case, such as:
The size of the stone
The location of the stone
The composition of the stone
Patient signs/symptoms
Medical Therapy
Most kidney stones do not require invasive treatment. In a patient who has a newly diagnosed ureteral stone <10 mm and whose symptoms are controlled, observation with periodic evaluation is an option for initial treatment. Patients who elect for an attempt at spontaneous passage should have well-controlled pain, no fever or evidence of infection, and adequate kidney function.
Drinking water
You should drink enough fluid — mostly water — to produce clear or nearly clear urine. Your doctor will likely give you a small strainer to urinate through, with the hopes that the passed stone can be collected for analysis. Straining your urine is crucial since once the stone is passed into the bladder and out of the body, it often does not cause pain.
Pain relievers
To relieve the pain from stone passage, your doctor may recommend pain relievers such as ibuprofen (Advil, Motrin), acetaminophen (Tylenol), or naproxen sodium (Aleve). In some cases you may need a stronger medicine such as Vicodin or Percocet.
Medical Expulsive Therapy
Your doctor may give you a medication to help pass your kidney stone. This type of medication, known as an alpha blocker, relaxes the muscles in your ureter, helping you pass the kidney stone more quickly and with less pain. This is especially helpful with stones in the ureter close to the bladder.
Surgical Therapy
Kidney stones that cannot be treated with conservative measures because of their size, location or patient signs/symptoms, or those that have failed to pass spontaneously with conservative measures, will need to be treated with a surgical procedure. The procedure that your doctor may recommend is based upon size, size location, and stone composition. These procedures are all considered to be minimally invasive, meaning that none require a significant incision.
Extracorporeal Shock Wave Lithotripsy (ESWL)
ESWL uses sound energy to create shock waves that fragment the stones into smaller pieces that can be passed through the ureter. It is used when stones are visible on a plain x-ray, which is used intermittently throughout the procedure to localize the stone. It is often used for stones in the kidney or high in the ureter. The procedure lasts 30 to 45 minutes and can cause moderate pain, so it involves light anesthesia/sedation to make you comfortable and limit movement during the procedure, which optimizes the efficacy of the lithotripsy. ESWL can cause blood in the urine, bruising on the back or abdomen, bleeding around the kidney and other adjacent organs, and discomfort as the stone fragments pass through the urinary tract. Your surgeon may place a stent in the ureter during the procedure to help facilitate the passage of the stone fragments.
Ureteroscopy
This procedure involves the passage of a thin fiber-optic telescope equipped with a camera through your urethra and bladder to your ureter. Once the stone is located, surgical tools can entrap the stone, or a laser fiber can be used to break it into small pieces that can be removed by the surgeon or pass in your urine. Your surgeon may place a stent in the ureter during the procedure to help facilitate the passage of the stone fragments to relieve swelling and promote healing. You may need general anesthesia during this procedure. This procedure is most effective in removing stones in the lower ureter near the bladder, or stones deemed to hard to fragment with ESWL.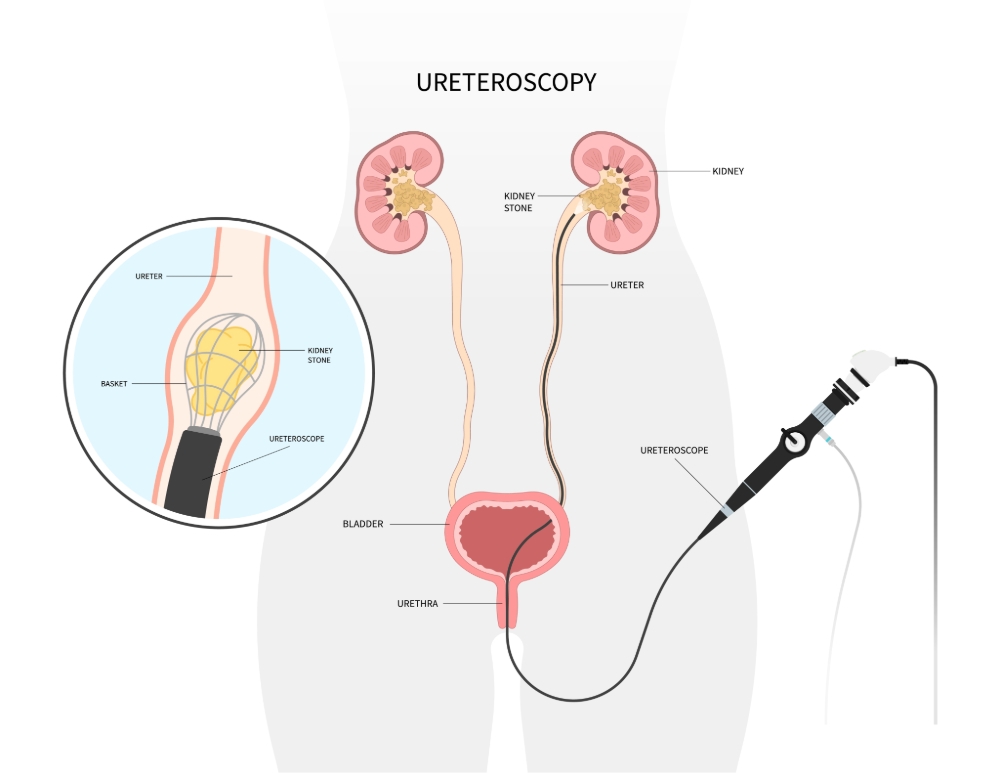
Percutaneous Nephrostolithotomy
This surgery may be recommended by your doctor to remove very large stones in the kidney. These stones are deemed too large to treat with ESWL or ureteroscopy. It involves removing a large kidney stone through a small incision (one inch) in your back using a fiber-optic telescope equipped with a camera. It involves general anesthesia and requires a hospital stay of one to two days to recover.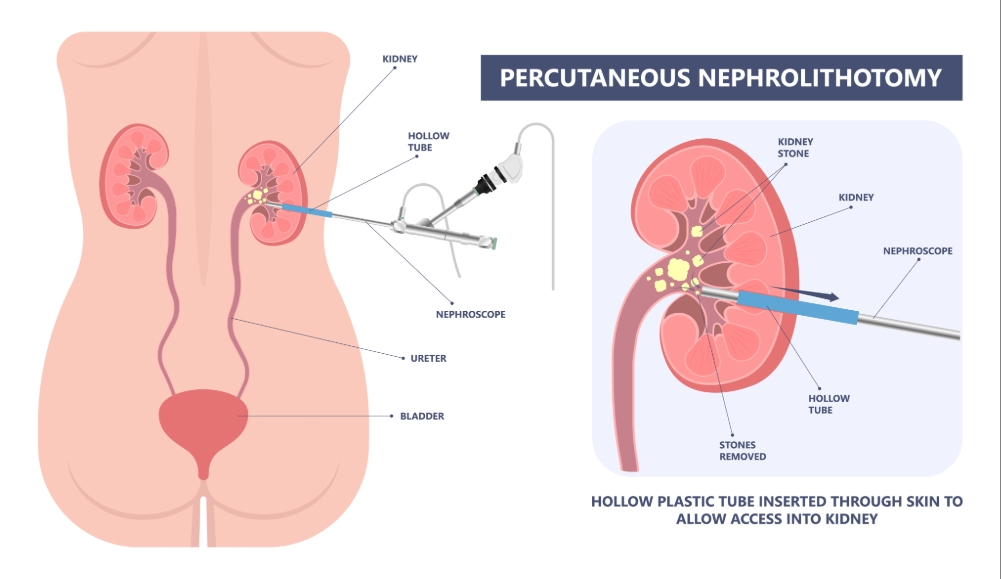
Emergent Therapy
In patients with obstructing stones who are showing signs of infection with fever, chills, fatigue, and/or kidney injury, urgent decompression of the kidney with either percutaneous drainage or a ureteral stent is needed in combination with appropriate antibiotic therapy. This will serve to unblock the kidney and treat the underlying infection. Definitive treatment of the stone should be delayed until the infection is resolved. Other indications for emergent therapy include bilateral kidney obstruction with kidney injury and unilateral obstruction with acute kidney injury in a patient with a solitary kidney.
Please call our office at (646) 962-9600 to schedule an appointment via phone. Our phone staff are available to help you Monday-Friday, from 9AM-5PM (EST).
If you'd like to learn more about each of our providers that specialize in Kidney Stone treatment, please view the "Our Care Team" page.