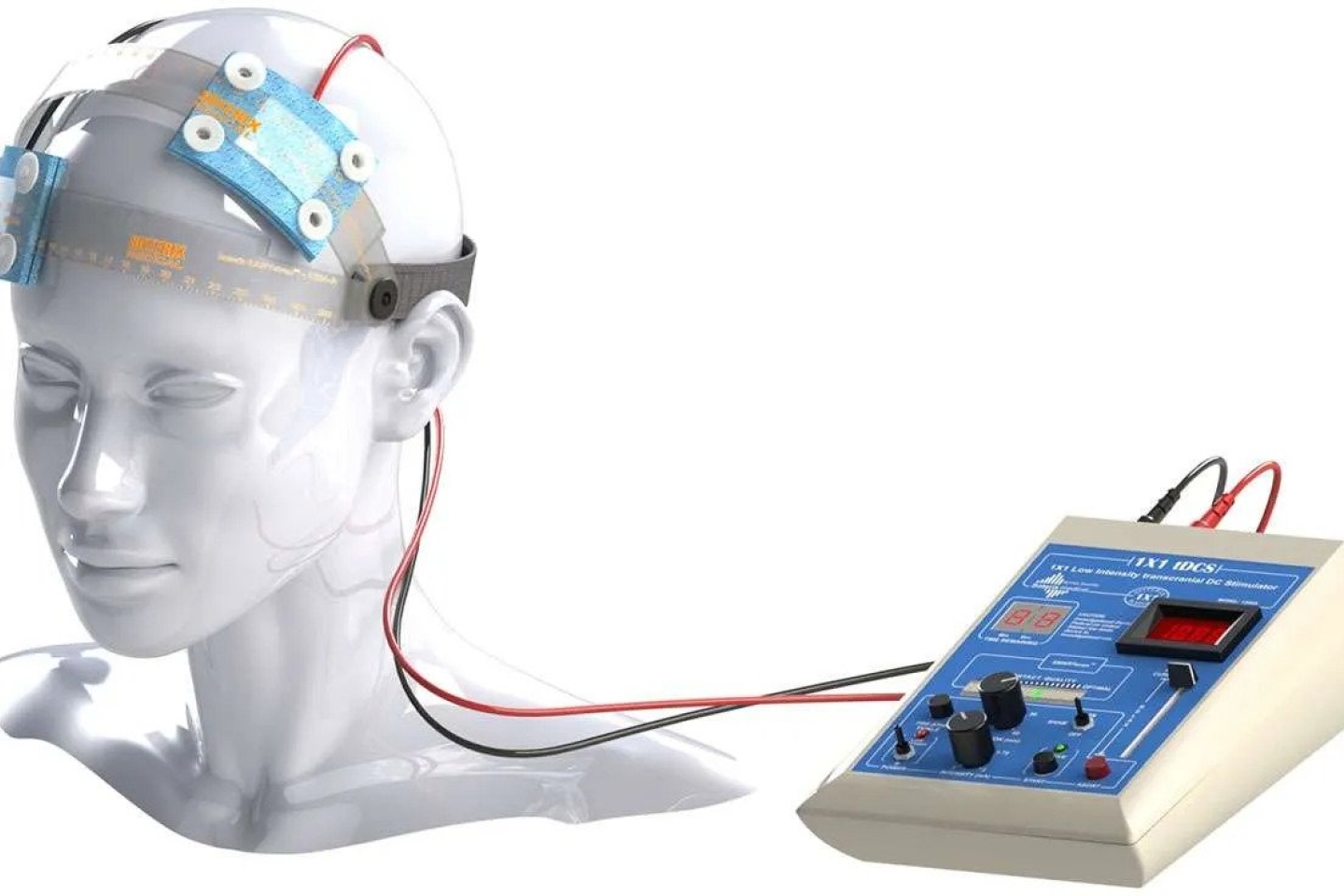
Transcranial direct current stimulation (tDCS) is a new, non-invasive technology that is being used in many areas of medicine. It is an electrical stimulation device with two electrodes, which are placed over specific areas of a patient’s head or neck, depending on individual needs. These electrodes deliver a very low-level electrical current that may influence the activity in your brain or spinal cord.
Think of the brain as active and “plastic,” able to learn a new skill or relearn one that has been lost due to traumatic brain injury, stroke or a movement disorder. A relatively new option being offered at Weill Cornell Medicine, tDCS can enhance the benefits of physical, occupational or speech therapy and hasten the return of lost skills, from language to movement, balance and everyday functioning.
And best of all, tDCS is designed to be used in the comfort and safety of your own home.
Dr. Joan Stilling, a specialist in general neurorehabilitation and Assistant Professor of Clinical Rehabilitation Medicine at Weill Cornell Medicine, uses tDCS for a variety of conditions that affect people’s ability to function, including:
Patients who have experienced a stroke and have ongoing fatigue or difficulties speaking, moving an arm or leg, or memory problems following their injury may benefit from tDCS therapy.
See Dr. Stilling’s answers to frequently asked questions about tDCS below.
There are many different tDCS devices available on the market. The typical device looks like a small rectangular electronic box. It has two spots where wires are inserted, allowing for connection to rubber electrodes that are placed on your head or neck. These electrodes are damp, as they’re soaked in salt water to allow a mild electrical current to flow from the device to a specific area on the surface of your head or neck.
We believe tDCS changes the level of excitability of neurons—the cells that help transmit important signals in the brain. The device can increase or decrease that level within specific parts of your brain for minutes to hours after stimulation. It has been seen to enhance the benefits of physical and occupational therapy, for example, when it’s applied while you are learning a new movement or skill or relearning one that requires rehabilitation. It’s a bit like having a cup of coffee to “wake up” a specific part of your brain and help it remember the skill you are trying to relearn.
The technology is usually well tolerated and has only mild side effects. Most patients report a slight itching, tingling, pins-and-needles or burning sensation under the electrode pads. This sensation usually dissipates after a few minutes. People may also experience a mild headache, dizziness or minor fatigue following treatment.
We determine the location based on the specific activity you’ll be doing when undergoing treatment. For example, if you’re focusing on walking, we’ll stimulate the part of your brain that’s involved in moving your legs. If you’re working with your therapist on speaking, we’ll stimulate different networks in your brain that have been shown to play a role in language.
We also take your medical history into account. For example, if you’ve had a stroke, we’ll look at your brain imaging and determine the optimal area to stimulate, given the size and location of your brain injury.
The tDCS device is considered very low-risk. Neither animal studies nor thousands of human research participants have shown any serious adverse events.
To be used at home, Weill Cornell Medicine’s tDCS therapy program is designed for patients who have a history of stroke, traumatic brain injury or a movement disorder. The tDCS program may help to improve your responsiveness to PT, OT or speech therapy. However, tDCS should not be used for anyone who has metal objects in their head area, eyes or neck. It also shouldn’t be used in patients who have another electrical device in their body, such as an implanted pump, stimulator or pacemaker. It can be considered for use with caution in people who have history of seizure or epilepsy.
If you’d like to learn more about tDCS or make an appointment with a rehabilitation medicine specialist, please visit here.