Robert De Niro. Colin Powell. Arnold Palmer. John Kerry. What do a celebrated actor, retired four-star general, golf legend, and near-POTUS have in common? They’ve all had prostate cancer and survived to tell their story.1
Prostate cancer is common and indiscriminate — it does not distinguish between celebrity figures and everyday men.
With roughly 180,000 to 230,000 new prostate cancer cases diagnosed in the U.S. each year,2,3,4 it’s critical that men (and the women who love them) are informed about this common but highly-treatable form of cancer. Read on to learn who’s at risk; the warning signs, causes, and treatments for prostate cancer; and when to see a doctor.
Here are the facts: Prostate cancer is the most common (non-skin) form of cancer in the U.S., affecting one in seven men during his lifetime.2 Prostate cancer is the second leading cause of cancer death among American men,2 and nearly 29,000 men in the U.S. will die of the disease each year.4
The good news is that most prostate cancers are slow-growing and highly treatable, especially when detected early. The five-year survival rate is almost 100 percent, with early detection, and 98 percent of men remain alive 10 years after their initial diagnosis.2
Understanding the function of the prostate and the importance of regular screenings can help men reduce their risk of developing prostate cancer and catch the disease early on. Let’s explore.
The prostate is a small, walnut-sized gland that sits under a man’s bladder. The gland is part of the male reproductive system and produces part of the seminal fluid, which helps carry sperm out of the body during orgasm. The prostate gland surrounds the urethra, the tube through which urine flows. When the gland becomes enlarged, it can make urination difficult — often the first sign of a prostate problem (but not necessarily indicative of cancer; more on that below).
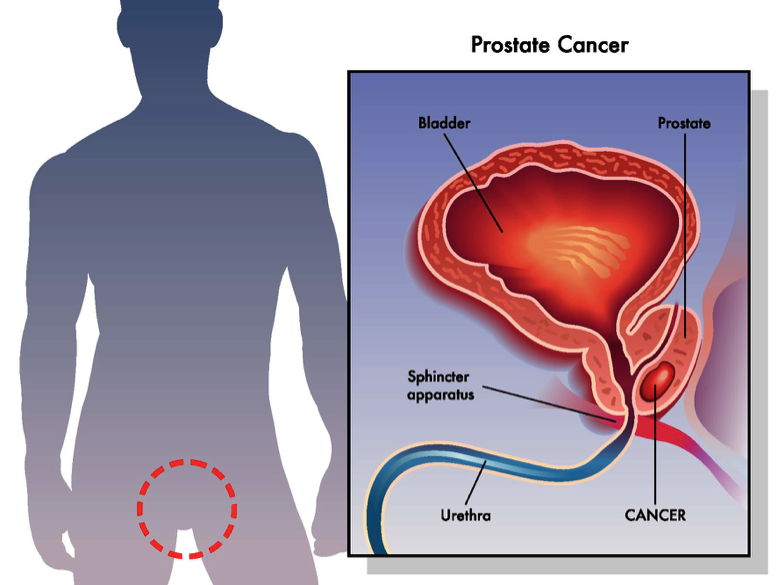
Like all cancers, prostate cancer begins in the cells of the body. Normally, cells grow and divide to form new cells, as needed, and old or damaged ones die and are flushed from the body. When there is a “glitch” in the process, new cells that aren’t needed may form, and old and damaged cells don’t die as they should — this build-up of cells forms a mass of tissue called a tumor.
Tumorous growths are either benign or malignant. Benign tumors are rarely life-threatening, often localized and non-spreading, and they can usually be removed without coming back. Conversely, malignant tumors sometimes pose a threat to life, can invade nearby organs and tissues, may spread to other parts of the body, and often grow back.
There are several factors that can influence a man’s risk for developing prostate cancer — some within his control and some not. These factors include:
Prostate cancer is a complex disease — in recent years researchers have come to understand that it’s really several diseases with different causes.2 Certain lifestyle factors, like smoking, low intake of vegetables in the diet, and obesity all may be risk factors for developing more aggressive forms of prostate cancer. Additional risks may include exposure to the chemical Agent Orange, lack of exercise and/or sedentary lifestyle, tall height, and high calcium intake.

Not all men will experience symptoms, especially in the early stages of cancer. Doctors are often the first to notice signs of prostate cancer during routine exams. Men rarely experience symptoms with early disease, however, which may include:

Because the prostate tends to get larger with age, some men may experience symptoms like difficulty passing urine as early as their 40s or 50s. Two common (non-cancer) prostate problems include:
Men may experience both of these problems at once, but one problem does not necessarily lead to another. No conclusive evidence exists that having an enlarged or inflamed prostate increases a man’s chances of developing cancer,5 and most prostate problems are not cancer.
There are four types of prostatitis:
Symptoms of prostatitis may include trouble passing urine and a strong frequent urge to go; chills and high fever; lower back pain/aches; pain in the belly, groin, or behind the scrotum; pressure or pain in the rectum and/or genital or rectal throbbing; painful ejaculation; and others.
BPH is a (noncancerous) enlargement of the prostate that constricts the urethra, blocking the flow of urine. Common symptoms of BPH include difficulty starting urination, weak or slow urinary stream, feeling of urgency to urinate, frequent trips to the bathroom at night, a urine stream that starts and stops, feeling of incomplete emptying of bladder, straining to urinate, and feeling the need to urinate again minutes after going.
The prostate gland produces a protein called prostate-specific antigen (PSA). When the prostate is inflamed, enlarged, infected, or affected by cancer, it releases higher-than-normal levels of this enzyme. Doctors can check for abnormal PSA levels with a simple blood test.
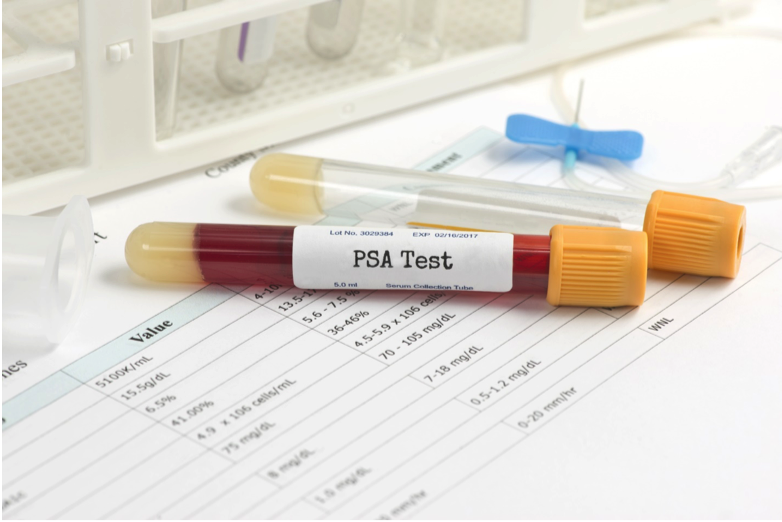
A digital rectal exam (DRE) can also reveal prostate issues. Many doctors perform the exam routinely as part of the annual physical for men of a certain age or those with certain risk factors.
PSA and DRE results are reported as a Gleason score. The higher the score, the more likely it is that prostate cancer has spread into nearby tissues.

Bone scans, CT scans, and MRIs are staging tests that can help show the extent to which prostate cancer has (or has not) spread into nearby tissues, organs, and bones.
Which treatment option a person’s doctor recommends will largely depend on the stage of the cancer, but may include:
If you’re experiencing any of the symptoms mentioned earlier, such as difficulty urinating, needing to go frequently, fever/chills, pelvic pain, a burning sensation while urinating, or recurring bladder infections, or other abnormal symptoms, see a physician right away.
Prostate cancer screenings have become routine for men over age 50 and high-risk candidates — and for good reason. The earlier prostate cancer is found, the easier it is to treat. Side effects like urinary incontinence and erectile dysfunction are also less likely with early-stage treatment. Talk to your physician about your individual risk, which is based on your age, lifestyle, family history, and other factors.

Cancer takes far too many lives in the U.S. and around the globe. See your doctor regularly to help ensure many years of good health to come with your loved ones.