A Weill Cornell Medicine-led research team has been awarded a 2024 Top 10 Clinical Research Achievement Award from the Clinical Research Forum in recognition of an influential 2023 New England Journal of Medicine study on early-stage lung cancer resection.
The award is one of 10 given annually by the Clinical Research Forum for highly innovative and clinically translatable research with the potential to provide major benefits to patients. The Washington, D.C.-based organization is an influential advocate for government funding of clinical research and the interests of American clinical research institutions generally. The winners will present their award-winning research April 4 at the Clinical Research Forum’s annual meeting in Las Vegas.
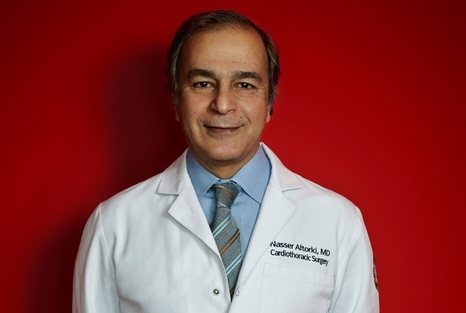
The clinical trial results were published Feb. 9, 2023 by a team led by Dr. Nasser Altorki, chief of the Division of Thoracic Surgery in the Department of Cardiothoracic Surgery at Weill Cornell Medicine and NewYork-Presbyterian/Weill Cornell Medical Center, and co-investigators from Duke University as well as investigators from 83 hospitals across the United States, Canada and Australia. The trial found that a surgery that removes only a portion of one of the five lobes that comprise a lung is as effective as removing an entire lobe for certain early-stage lung cancer patients.
“This award means a lot to me, as it recognizes an important advance in the surgical treatment of patients with early-stage lung cancer,” said Dr. Altorki, who is also the David B. Skinner, M.D. Professor of Thoracic Surgery and a professor of cardiothoracic surgery at Weill Cornell Medicine, and a thoracic surgeon at NewYork-Presbyterian/Weill Cornell Medical Center. “I think the award also recognizes the contribution of Weill Cornell Medicine and NewYork-Presbyterian to cooperative group trials supported by the National Cancer Institute.”
In the trial, investigators compared outcomes for nearly 700 patients with early-stage lung cancer, about half of whom were randomly assigned to “lobectomy” surgery, which removes the whole lobe, while the other half had “sublobar resection” surgery, which removes part of the affected lobe. Over a median follow-up period of seven years after surgery, the two groups did not differ significantly in terms of disease-free or overall survival, and the sublobar group had modestly better lung function.
Lobectomy has been the standard approach for early-stage lung cancer surgery for almost 50 years, but the study’s results indicate that a subset of early-stage lung cancer patients would be better off, or at least no worse, with the more tissue-conserving sublobar surgery.
“We started the trial in 2007 and it took about 10 years to complete,” said Dr. Altorki, who is also a member of the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine. “We then we had to wait until we got the results, which unexpectedly came in May of 2022. They were amazing results, and it was worth the wait, and it changed practice.”