
With the COVID-19 pandemic coinciding with the start of spring, you may be wondering when your respiratory symptoms indicate allergies – or something more serious. Dr. William Reisacher, associate professor and director of allergy services in the Department of Otolaryngology – Head and Neck Surgery at Weill Cornell Medicine, and an associate attending otolaryngologist at NewYork-Presbyterian/Weill Cornell Medical Center, explains how to identify the warning signs of COVID-19 that may be a reason to give your doctor a call.
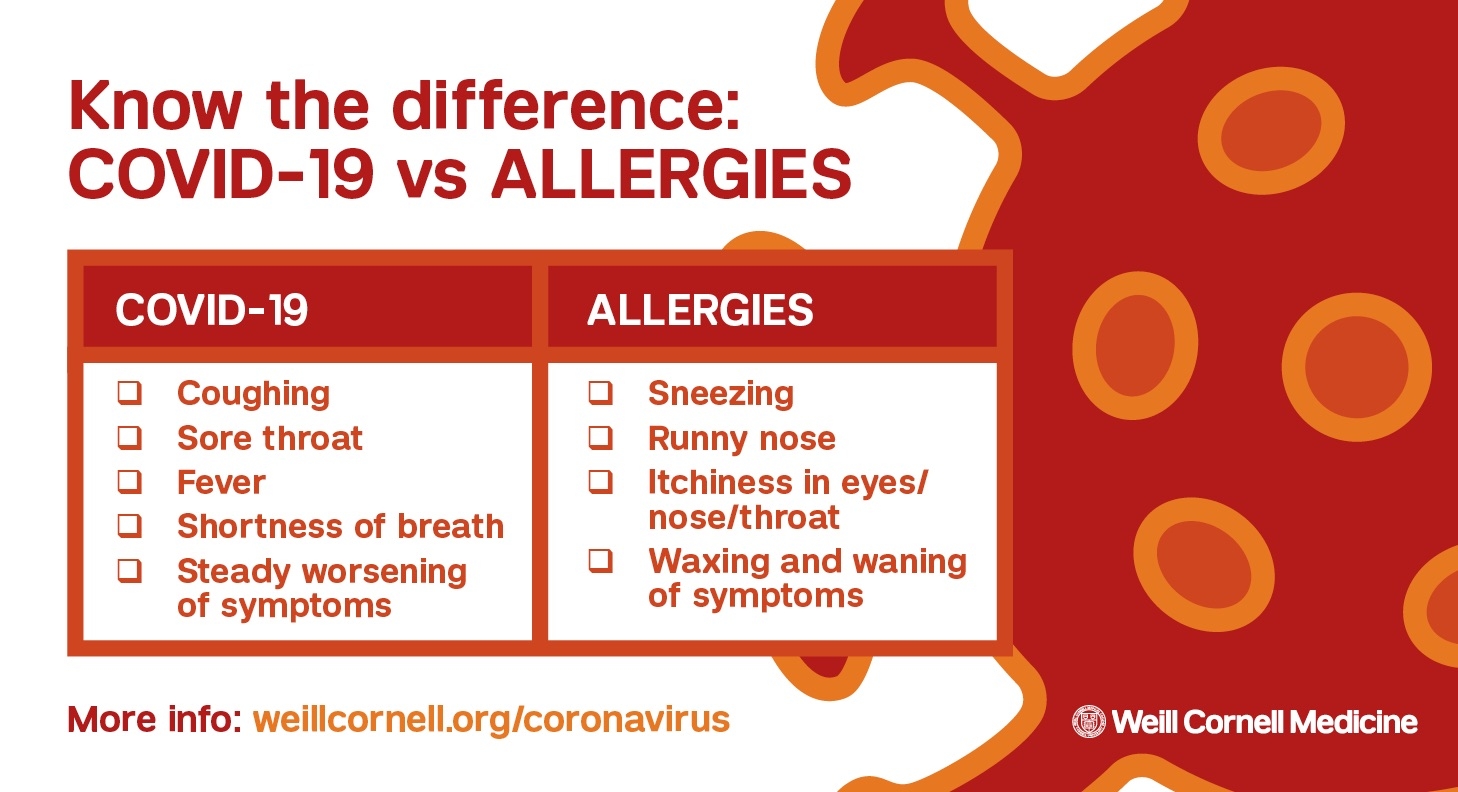
In both cases the lungs and throat might be affected, but with a viral illness there is fever—and that’s not present with allergies. Allergies to pollen and grasses cause sneezing and itchiness in the eyes, nose and throat, but you would not see those symptoms from the novel coronavirus. Cough is a common symptom of COVID-19, which can also be present in some patients with allergies.
Here’s another difference: With seasonal allergies, the symptoms tend to wax and wane and get worse when you are outside. With a viral infection, there’s typically a steady worsening.
Kids with allergies tend to be restless, while with adults who have allergies, there’s more fatigue. We’re still learning about the differences between how grownups and kids experience COVID-19, though in general children seem to have less severe symptoms. If a child is lethargic and feverish and has a persistent cough, in the absence of itchy eyes and a runny nose, then you should call the pediatrician.
At this point, we do not know. While people with compromised immune systems are at higher risk of severe COVID-19, people with allergies don’t have a compromised immune system; their allergies are actually an overreaction of the immune system.
That said, among people with some degree of asthma, those with worse disease tend to be in a higher-risk group for viral infections, particularly if the asthma is not well managed. So this is a good time to review the way you are managing your allergies – and your asthma, if you have it. During a virtual visit, you and your doctor can go over the ways you are managing your condition and make any modifications if needed.
No, although it’s smart to be prepared. If you’re dealing with food allergies, make sure you have a good supply of the right foods, and have a second EpiPen on hand in case you need it—no need to stockpile, though!
The same goes for asthma; make sure you have an extra inhaler. In general, patients should make sure they have enough medication to tide them over in case they run out and can’t refill their prescriptions right away.
With any viral infection, doctors have to pay attention to the risk of aerosolization. But inhalers can be used safely by a patient, and they should be used when they are needed, whether you are at home or outside. If you have to use inhalers, however, it’s still very important to give extra distance when around other people.
At Weill Cornell Medicine, office visits are available on a limited basis, for urgent situations only. However, policies may differ based on the doctor and the office, so it’s best to contact your allergist and see if they are still giving injections at this time. The current guidelines are recommending that people older than 65, or those with underlying medical problems, should stay at home unless absolutely necessary. Patients can also be seen through online video visits, which are becoming very popular during this crisis.
If your allergy is due to pollen, being inside may be helpful, and if spring cleaning makes you feel better, that’s a benefit. Do keep in mind that cleaning can kick up a lot of dust, so if the issue is indoor allergens, get some clarification from your doctor—during a video visit, of course.
All of us at Weill Cornell Medicine understand that this is a difficult time for all New Yorkers. As experts in immunology, pulmonary medicine, and critical care medicine, we are working diligently to provide the greatest possible care to patients in need.
We are available to all New Yorkers who have questions or concerns. Please call our hotline at (646) 697-4000 for information about COVID-19 or read our patient guide.