Hypospadias is a condition where the opening in the penis is not at the tip of the penis. The penis begins to form in the sixth week of fetal life. During this time, two folds of tissue join each other in the middle and a hollow tube (urethra) is formed in the middle of the future penis. Any interruption in this process leads to the opening being located further from the end of the penis.
Hypospadias is usually classified according to the location of the opening. These types based on the opening’s location include:
As hypospadias increases in severity, the opening can be further back on the penis. The most severe types can have openings at the region of the scrotum or between the anus and scrotum. Hypospadias can also be associated with chordee, a condition causing the downward curvature of the penis. Both hypospadias and chordee must be repaired to restore urinary and reproductive health. 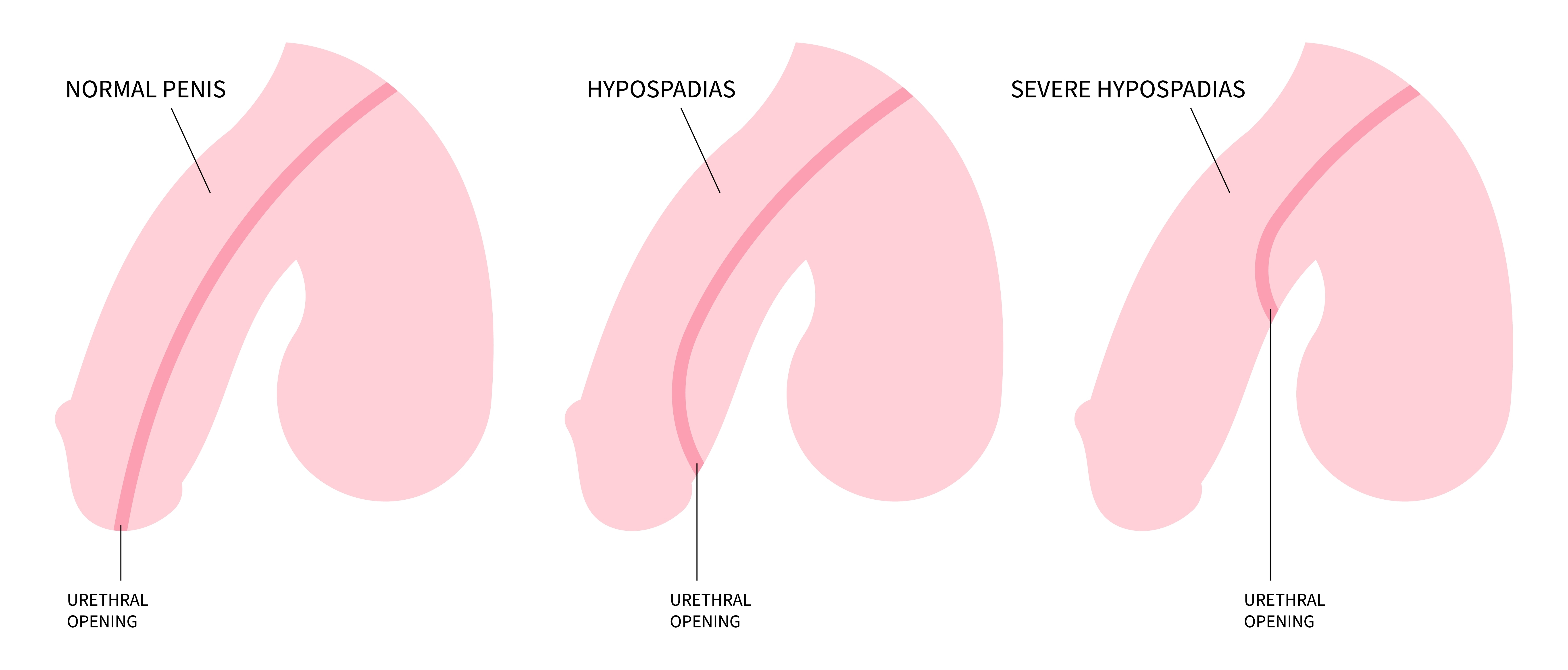
The most common symptom of hypospadias is the opening of the urethra being in a different location other than the penis’ tip.
Other symptoms may include:
The exact cause of hypospadias is unknown. With that said, some potential risk factors include:
There is no exact way to prevent hypospadias. However, it is important to identify any family history of this condition or genetic susceptibility. Additionally, it is important to avoid certain chemicals or hormones when pregnant to limit the risk of developing hypospadias.
Hypospadias is usually diagnosed when a child is born. At this time, if circumcision is considered for the baby, it is important to delay this procedure until the child is seen by a urologist as the foreskin can provide essential skin that is needed to reconstruct the urethra.
Ultimately, hypospadias is repaired through surgery under general anesthesia. While the repair is typically done before a child turns one-year old, the exact age of repair can vary according to the size of the penis and severity of the defect. During the procedure, the urethra is extended to the tip of the penis to its normal location. Any bend will also be straightened, which will allow the child to stand while urinating as well as have typical reproductive health and sexual function. With most, a small tube, or “stent,” will exit the tip of their new meatus to protect the new urethra and allow for adequate healing.
The exact type of surgery depends on the severity of hypospadias.
Most patients leave the hospital the same day, or the following day, after a hypospadias repair. However, more complex repairs may require longer hospital stays due to the need for bedrest and immobilization immediately after the operation. The team at WCM has been able to repair most children with a single operation, but on occasion, a second operation may be needed.
Potential Treatment Complications
The most common complications from hypospadias repair include fistula and stricture. A fistula occurs if a hole develops along the underside of the penis, which may lead to urine leakage. A stricture is a scar that can form leading to the narrowing in the urethra. If either of these occur, an additional repair, usually six months later, will be needed.
Additionally, use of antibiotics during and after surgery helps decrease the risk of infection. Bleeding is also controlled by using a “penile tourniquet” during the operation, limiting blood loss while still allowing the surgeon to see the tissue.
After hypospadias repair, the child will have a few follow-up appointments with the urologist to remove any tubes and to check in on the recovery process. Regular follow-ups are then suggested with a pediatric urologist to ensure there are not complications as the child enters their toddler and teenage years.
To request an appointment or learn more about our program, please call our office at (212) 746-5337. Our phone staff is available Monday through Friday, 9 AM to 5PM (EST).
Meet our expert providers who specialize in Hypospadias: