
This patient story originally appeared on Department of Neurological Surgery.
You might know the name Dr. Orna Guralnik from having read one of her features in The New York Times or The Washington Post, or you may have seen her profiled in The New Yorker. It’s even more likely that know of her as the host of the award-winning documentary series Couples Therapy on Showtime. She’s a TV host, therapist, writer, celebrity, working mom — in other words, she’s extremely busy. “I’m a typical New Yorker,” Orna laughs. “I basically work, or I’m with my two kids, 24/7. Apart from yoga, my schedule’s incredibly packed.”
But what happens when back pain starts interfering with those tightly packed appointments and obligations?
“I started feeling this pain at the bottom of my spine,” Orna recalls. “It would hurt at night and it would wake me up. I was tired from the pain, but I worked through it. The main thing it affected was my yoga practice — it really constricted what I was doing and I worried that I was damaging myself. I saw physical therapists and did some exercises that did absolutely nothing. Doctors I visited thought I was just complaining. It felt dismissive, like, ’You do yoga, so your back will obviously hurt.’ But something just felt strange. Finally, I went to a rheumatologist and asked him if he could get me an MRI since everyone was denying me one.”

A pre-operative MRI scan revealed that Orna had a tumor on her spine, but it could not provide more precise information about it.
Her persistence paid off when the MRI revealed that Orna had a spine tumor. “Everyone was alarmed,” she recalls. “A good friend of mine worked with someone at NewYork-Presbyterian Weill Cornell Medicine, so I asked them to find me the best doctor there. They recommended Dr. Roger Härtl.”
It was an excellent recommendation. Dr. Härtl, a co-director of Och Spine at NewYork-Presbyterian at the Weill Cornell Medicine Center for Comprehensive Spine Care, is one of the most respected spine surgeons in the world. He is well known as an expert clinician, and also as one of the most technologically advanced spine surgeons anywhere.
“We treat spine tumors every day here, and we always start with the basics,” says Dr. Härtl. “We identify its primary location, see if there are other lesions, and then try to determine whether it is benign or malignant. Looking at her scans, we strongly felt that the tumor wasn’t cancerous; we leaned towards a diagnosis of a schwannoma – a benign tumor. However, we’d only know for sure when we operated. We had to act and remove it in its entirety before it would grow even bigger.”
An unexpected surgery is never easy, but in Orna’s case her job made things especially complicated. Still, she found comfort in Dr. Hartl’s approach.

Using augmented reality (AR) in the operating room requires specialty equipment as well as highly trained personnel.
“Going into surgery meant we had to stop production on the show,” she says. “A lot was happening. I was scared about having someone operate on my spine – and about what they would find. But Dr. Härtl was very sweet, and there was something warm, reassuring, and open about his demeanor. He didn’t promise me things that he couldn’t promise. He explained what the plan was and took the cue from me that I really wanted to understand the details of what was going on. It was really important to me that he was willing to go into the details of the procedure and the technology they would use.”
Dr. Hartl explained that he’d be using augmented reality in the operating room – an emerging technology that allows for greater precision in locating and removing a spine tumor.
“We are at a new frontier in the science of spine surgery,” Dr. Härtl says. “In today’s operating room, we pair our surgical skills with new technology to perform more advanced, minimally invasive techniques. Augmented reality, or AR, helps us fine-tune our accuracy. On a macro level, that allows us to extend minimally invasive surgery towards more and more types of surgeries. And on a micro level, the increased precision AR affords us in the operating room means smaller incisions – and that translates to less risk overall and a faster recovery for the patient.”
Just two weeks after her initial meeting with Dr. Härtl, Orna’s husband and son dropped her off at NewYork-Presbyterian/Weill Cornell Medical Center. Her daughter and mother stayed with her until she went into the operating room.
“Orna’s surgery was greatly enhanced by the use of augmented reality,” says Dr. Härtl. “Using the pre-surgical scans as a guide, we were able to navigate to the vicinity of the tumor. Once we confirmed the mass was indeed a schwannoma, we were able to remove it completely with the assistance of AR, reducing the amount of disruption in the muscles in her back to get there. Overall, this approach optimized Orna’s safety and recovery after surgery.”
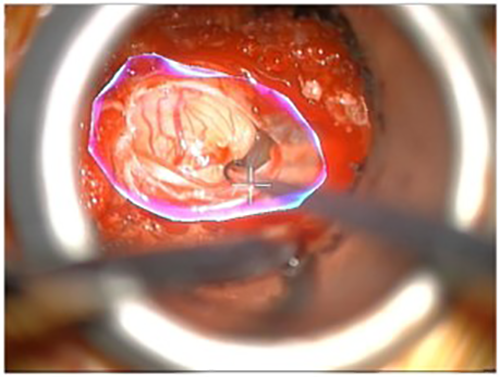
Augmented reality allows a neurosurgeon to visualize the margins of a tumor even when they are not visible to the eye. In this case the white area at center is the visible tumor; the AR outline shows how much larger the tumor is.
“I’m a technology geek, so when Dr. Härtl told me about using AR in my surgery I just loved it!” exclaims Orna. “Prior to the surgery I was worried about the possibility of an errant cut damaging my spinal cord. But knowing about the technology in Dr. Härtl’s capable hands helped ease my concerns. What was more impressive was seeing them perform my surgery later via a recording. It felt like sci-fi; it was fun.”
No technology can make spine surgery itself fun, of course, and Orna had a typically uncomfortable first post-operative day. “I was glad to wake up and not be dead,” she says, “but it was 24 hours of nausea hell and some pain. It was uncomfortable, but it cleared up, and after a couple of nights I was cleared to go home.”
Dr. Härtl’s team had estimated that Orna’s recovery would take six weeks, and her family pulled out all the stops in preparation. “My mom came to help with the kids, but she only stayed for four days,” says Orna. “There was a lot of preparation for an intense recovery, but it was a lot less than I thought. After a few days of feeling lousy from the anesthesia, the swelling, and the pain, it was a pretty fast healing curve. After two weeks, I felt fine enough to fly out to Los Angeles, where Showtime was having a big Christmas celebration for Couples Therapy. Everyone thought I was completely crazy to go!”

Just two weeks after surgery, Orna was on a plane to Los Angeles for a Showtime party celebrating Couples Therapy. Today she feels great and is glad she spoke up for herself. Photo: Sean McGinty, courtesy Showtime
Orna returned to her regular routine, and show tapings resumed. “The only thing that took a long time was getting back to my yoga and my exercise practice,” she says. “My back was stiff, but I don’t think there was any way around that. It’s gone now, and I barely have a scar.”
With the experience behind her, Orna says she feels great and is glad to put it all in the past. She is especially glad she didn’t accept the word of doctors who didn’t take her seriously. After all, she knows herself better than anyone, and she knew something was wrong.
“Today, I’m back – my life is very, very full,” she says. “I’m really glad I insisted on the MRI and that I didn’t listen to my previous doctors. I felt mad that they were dismissive. But I would tell anyone who was in the same position as I was to get the best doctor you can – and get the surgery done as soon as you can.”