What is rejection?
Rejection is a normal reaction of the body to a foreign object. When a new kidney is placed in a person's body, the body sees the transplanted organ as a threat and tries to attack it. The immune system makes antibodies to try to kill the new organ, not realizing that the transplanted kidney is beneficial.
To allow the organ to successfully live in a new body, medications must be given to suppress the immune system from attacking the organ for as long as the transplant continues to function.
If rejection does occur, it can be successfully treated in many cases, especially when caught early. This is why it is very important to take all medications as directed and follow-up with our transplant center as instructed.
Even if rejection does not cause the kidney to fail immediately, it can permanently damage the kidney and shorten its lifespan.
What are the risks of kidney transplantation?
There are several categories of risks that may be seen with kidney transplantation.
The first are risks surrounding the surgery itself. These risks include side effects of general anesthesia; bleeding; blood clots; leaking or blockage of the ureter (tube that carries urine from the kidney to the bladder); infection; failure of the transplanted kidney to work; rejection of the kidney.
Other risks come from the medications that must be taken to prevent rejection of the kidney. These may include high blood sugar or diabetes; high blood pressure; electrolyte imbalance; skin changes; weight gain; nausea, vomiting or diarrhea; thinning of hair. Patients taking immunosuppression are also at higher risk for developing infection and cancer, particularly skin cancer.
What can I expect when my child gets a kidney transplant?
If all goes well and your child is designated to receive the kidney transplant, the surgery takes about 2 to 4 hours.

For pediatric patients with complex genitourinary anatomy, the surgery may take longer if the child requires urologic surgery at the same time as their transplant.
In most cases, the diseased kidneys are left in place during the transplant procedure, although some children require removal of one or both of their native kidneys at the same time as their transplant. The transplanted kidney is placed in the lower abdomen on the front side of the body.
Read more about the kidneys and how they work.
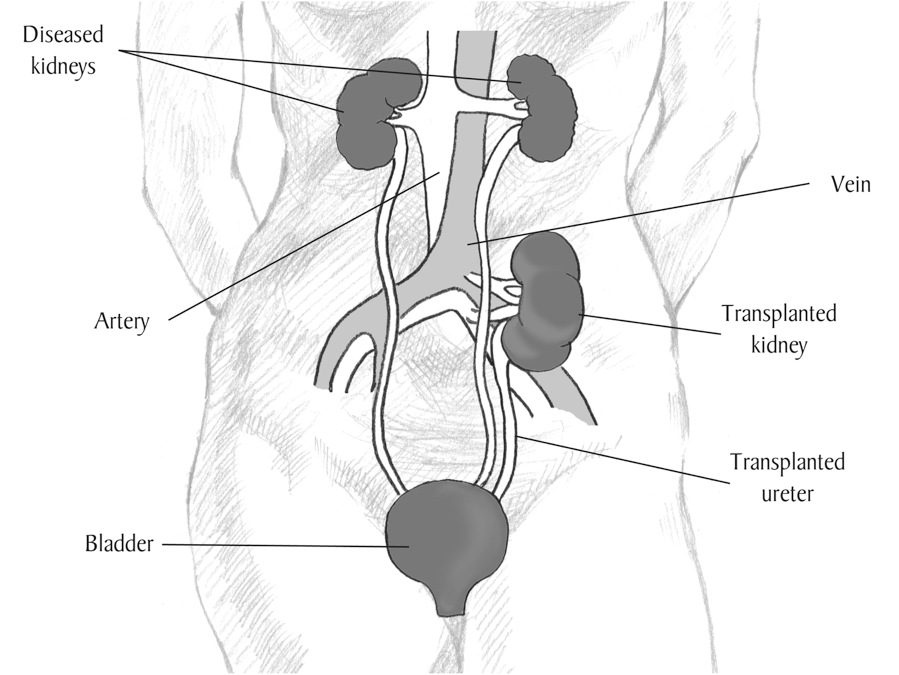
Image courtesy of the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health
The transplant is performed under general anesthesia, and after the surgery, your child will be transferred to the Pediatric Intensive Care Unit (ICU) for close monitoring.
Most children remain in the hospital for 4 to 7 days after their kidney transplant. Your child’s recovery period will consist of having his/her diet advanced, getting out of bed to walk, and participating in educational sessions with nurses, pharmacists, nutritionists, social workers, and others.
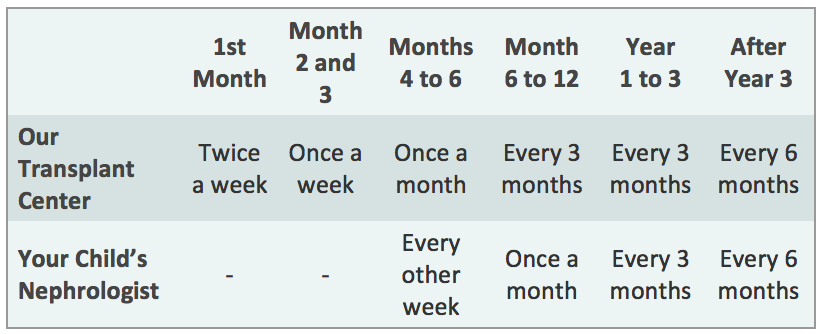
After your child is discharged from the hospital, you should expect to come back to the transplant clinic 2 to 3 times a week for the first month, then weekly for the next two months, then less frequently, depending on how your child is doing.
Your child will also be able to return to the kidney doctor who was caring for them before their transplant. We will work closely with your child’s doctor to manage their transplant, and you will continue to visit our Transplant Center periodically to ensure that your child’s kidney is functioning well, according to the schedule below. However, more frequent visits to the transplant center may be needed depending on your child’s post-transplant course.
How am I notified when a kidney is available for my child?
Each transplant team has their own specific guidelines regarding waiting on the transplant list and being notified when a donor organ is available.
In most instances, you will be notified by phone that an organ is available. You will be told to come to the hospital immediately so that your child can be prepared for the transplant. Even if you are called into the hospital, it does not guarantee that your child will receive that kidney; sometimes the kidney may go to someone higher on the list at another center. In addition, there may be a reaction when the donor's blood is mixed with your blood (called a positive crossmatch), which may indicate that your child should not receive that organ due to high risk of rejection.
Is living donation an option?
We all have heard about the shortage of organs available for transplantation. Unfortunately, the number of deceased donor organs has remained stagnant over the last several years, and this trend is expected to continue. As can be seen from the facts below, there is a great need to increase transplant opportunities for patients with kidney disease.
Although the 16,000+ kidney transplants performed each year in the United States may sound like a lot, the number is small compared to the number of people who are on dialysis, which is more than 650,000. It is also quite small when compared to the number of people waiting for a kidney (more than 95,000) and those never even referred for transplant evaluation (130,000+).
Given the high rate of complications and death while on dialysis, an increase in living donor kidney transplants holds the hope for improving the ability to transplant people who need a kidney.
Benefits of Living Donor Over Deceased Donor Kidney Transplantation
In addition to increasing the number of kidney transplants, living donation also provides the following benefits:
• Ability to schedule the transplant at a time that is convenient for both the donor and recipient helps to facilitate pre-emptive transplantation (transplant before the recipient needs dialysis), which is associated with better outcomes for the recipient
• Superior quality of living donor organs (as compared to deceased donor organs) leads to:
• Better function of the transplanted organ (immediate in the overwhelming majority of cases)
• Longer survival of the transplanted organ

I have a different question.
Please contact us if you have other questions not addressed here.
We are happy to answer them for you and will be happy to post them on this website for the benefit of others who may have the same question.
We can be reached at livingdonorkidneycenter@med.cornell.edu.
I want to donate to someone in the United States but live outside of the U.S. Is that possible?
It is possible to donate to someone who lives in the United States if you live outside of the U.S.
However, this ability varies greatly depending on where you live. In addition, this option is generally limited to donations to a blood relative.
It tends to be a slow process. First, you must go to your local doctor and have your blood type and other basic laboratory values checked, have a chest X-ray, have your medical history recorded, and a physical exam performed. The results of these tests are then sent to the transplant center in the United States, where they are reviewed.
If it looks like you are suitable to be a donor, the transplant center will generate a letter to assist you with your visa application. You are responsible for the rest of your visa application. If a visa is granted (usually for a 3 month time period), then the final testing and planning for the surgery can begin.
Will I have trouble obtaining health insurance in the future?
In some cases, having been a kidney donor can impact the donor's ability to obtain both health insurance and life insurance. Therefore, it is highly recommended that people considering donation obtain these types of insurance prior to becoming a donor.
Are there any expenses related to donation that aren't covered by my recipient's insurance?
Yes, there are "out-of-pocket" expenses that are not covered by insurance. These include expenses related to travel and hotel stays, childcare, elder care, follow-up costs (depends on where follow-up occurs (at transplant center or with your own doctor), and lost wages.
Your recipient is allowed by law to assist you with these types of expenses. In addition, there are assistance programs and tax deductions available related to these out-of-pocket costs that you might incur as a living donor.
Does the insurance coverage work the same way if I choose to be an altruistic donor or participate in donor exchange?
Yes, the insurance coverage provided by the recipient's insurance works the same way. Any logistics related to the insurance coverage (for example, if the donor is being worked up at a different transplant center than the recipient) are managed by the transplant centers.