Melanoma is a type of a skin cancer that occurs in melanocytes, the cells that give the skin its color. When these cells grow out of control, melanoma can form.
Melanoma is currently the 4th most common cancer in U.S. adults. If melanoma spreads beyond the skin to other parts of the body, it’s considered advanced melanoma.
We spoke with Dr. Paul Chapman, a medical oncologist at Weill Cornell Medicine/NewYork-Presbyterian Hospital with over 35 years of experience in melanoma care and research, to discuss important information patients should know about how this type of skin cancer.
Melanoma most commonly starts developing within skin that’s frequently exposed to ultraviolet (UV) light from either the sun or tanning lamps. In more rare cases, melanomas can also form in the eyes or mucous membranes. UV exposure can damage a cell’s genetic makeup, or DNA, which can affect how those cells grow and divide. When your skin’s DNA is damaged, the cells can reproduce rapidly, leading to melanoma.
Anyone can develop melanoma, but overexposure to sunlight and sunburns are a major risk factor. Other risk factors include a family history of melanoma, fair skin, light eyes, a history of tanning bed use, and having a surplus of moles. Melanoma is more common in white people, but it can occur in people of all skin types.
Changes in an existing mole or developing a new pigmented or unusual looking spot on the skin can be a sign that melanoma has formed. This can occur anywhere on the body, but melanomas are most often found in the arms, back, face, and legs, as these areas are more frequently exposed to the sun.
Typical moles are most often a uniform color, which could be pink, tan, black, or brown. Moles that are asymmetrical in shape, change color or size, become itchy or bleed, or have an unusual border may indicate melanoma.
There are a variety of treatment options for melanoma depending on the stage of the melanoma, if it has spread to other areas, and your overall health.
Surgery is the main treatment option for most melanomas. If melanoma is caught in an early stage, surgery alone may be a possible cure. If the melanoma has spread, a combination of surgery, immune checkpoint inhibitors, targeted therapies, chemotherapy, and/or radiation may be used.
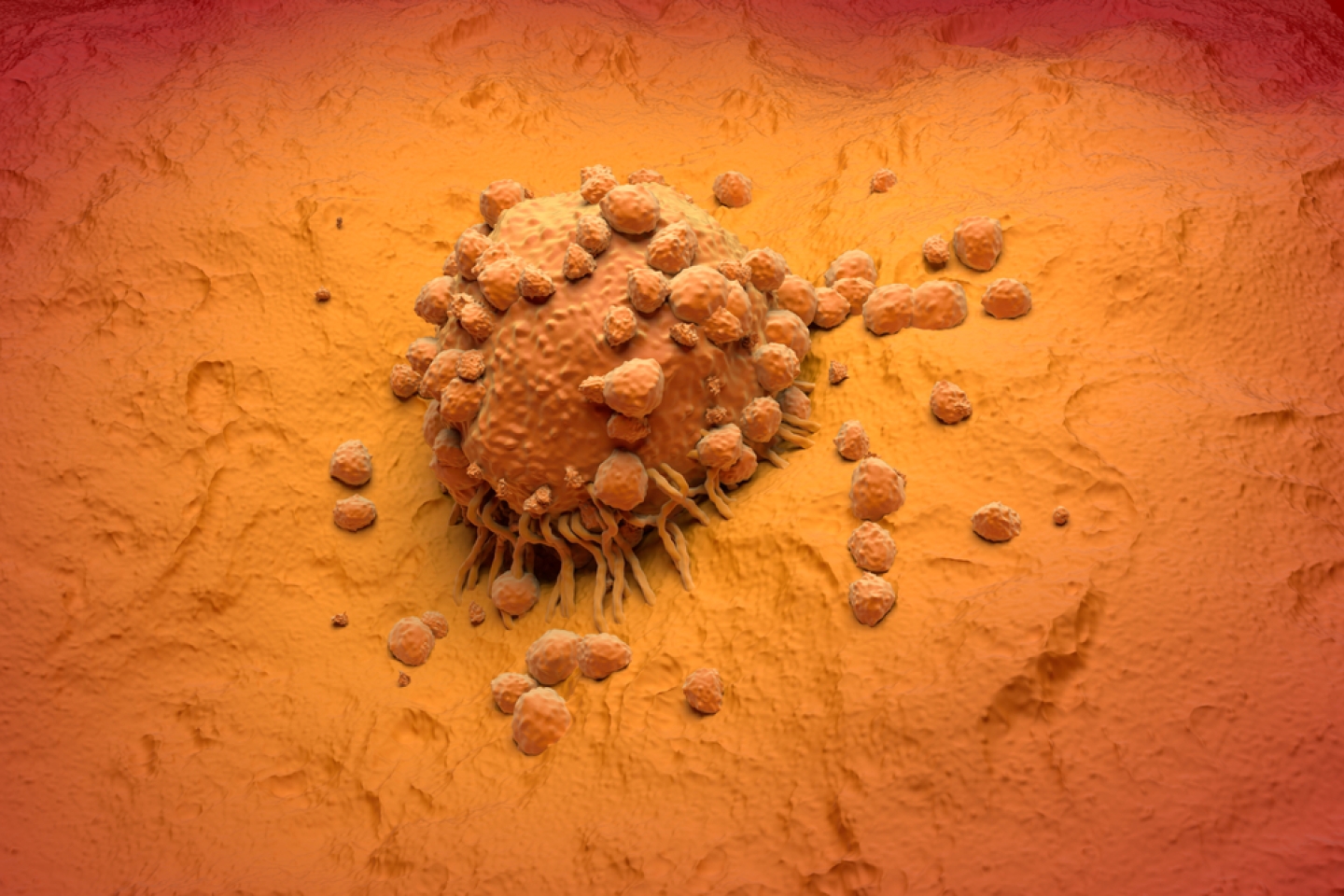
Immune checkpoint inhibitors work by targeting “checkpoint” proteins in the body in order to help the immune system attack the melanoma cells. These “checkpoint” proteins are like switches that need to be turned off in order to activate the immune system against cancer cells. There are a number of immune checkpoint inhibitors approved for the treatment of melanoma. Sometimes they are used alone, sometimes in combination.
Targeted therapies target mutations in specific genes that cause the cancer to grow. These treatments work by specifically targeting these cells and inhibiting their growth while leaving normal cells alone.
Chemotherapy works by targeting rapidly dividing cells in the body, including cancer cells. Chemotherapy travels through the blood to all parts of the body and can be used in more advanced melanoma that has spread beyond the skin.
Radiation therapy uses high-energy rays to kill cancer cells. It may be used when melanoma has spread to other parts of the body or after surgery to lower the risk of the cancer coming back.
Tumor-infiltrating lymphocyte (TIL) therapy is a new form of cellular immunotherapy that is used to treat advanced melanoma that hasn’t responded to other forms of treatment. TIL therapy uses a patient’s own immune cells to target cancer cells. Weill Cornell Medicine is proud to offer this innovative therapy to our patients.
Clinical trials are aimed at discovering new drugs or therapies that are not yet approved by the United States Food and Drug Administration (FDA). Enrolling in a clinical study may be the best treatment option for some patients after an initial melanoma diagnosis or after other treatment options have not led to a positive response against the cancer.
It’s important to be aware of changes to your skin and to perform regular self-skin exams. Typically, dermatologists recommend annual skin checks and monitor for changes during these visits. Additionally, if you see any areas that appear abnormal or have changed appearance since you last examined them, reach out to a health care professional for a more thorough exam.