
This story originally appeared on our Division of General Internal Medicine website.
People who felt lonely before having a heart attack were significantly more likely to end up back in the hospital within a month of discharge, according to findings by the researchers in the Division of General Internal Medicine at Weill Cornell Medicine. The study, published Dec. 2025 in the Journal of Medical Care, suggests that feeling lonely — independent of other health or social factors — can meaningfully affect recovery after a heart attack.
Loneliness is widespread, affecting nearly two-thirds of U.S. adults, and has increasingly been recognized as a serious public health concern. Recent advisories from the U.S. Surgeon General and the American Heart Association have emphasized its harmful effects, including its association to heart disease, yet its impact on short-term outcomes after AMI hasn’t been entirely understood. The researchers used data from the national REGARDS study to explore this relationship.
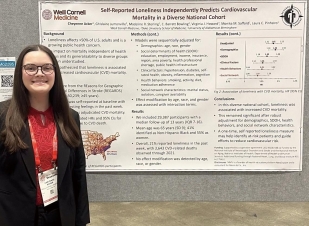
Cheyenne Acker
The study was led by Cheyenne Acker, a fourth-year medical student, Orysya Soroka, senior research data analyst, Dr. Madeline Sterling, associate professor of medicine, Dr. Parag Goyal, associate professor of medicine, Dr. Monika Safford, professor of medicine and Dr. Laura Pinheiro, associate professor in the Division of General Internal Medicine at Weill Cornell Medicine.
They focused on 749 Medicare beneficiaries who survived an adjudicated acute myocardial infarction (AMI). Participants had an average age of 77, and one in five reported feeling lonely. Within 30 days of hospital discharge, 29% of patients experienced an emergency department visit or hospital readmission. These patients had a 61% higher risk of emergency visit or readmission. Even after accounting for demographic and medical factors such as age and health conditions, loneliness was still associated with about a 48% higher risk of readmission or emergency visit.
These findings suggest that loneliness, even when measured years before a heart attack, can help predict short-term health care utilization. “Loneliness isn’t just emotional, it has real consequences for heart attack recovery,” said Cheyanne. The study highlights that incorporating assessments of social health into discharge planning may help reduce avoidable readmissions, a key priority in national strategies to improve post-AMI quality of life.
As loneliness continues to affect millions of Americans, this study offers important insight into how social factors shape recovery after major cardiac events and where targeted support may make a meaningful difference.
This work was supported by the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institute on Aging (NIA) of the National Institutes of Health, Department of Health and Human Services. Additional funding was provided by the National Heart, Lung and Blood Institute (NHLBI).